See all "Menstruation" Section Topics
Yeast infections can happen at any time, but for some women, they find that their period indicates a time when they are likely to develop vaginal Candidiasis. It has long been known, that the hormones which regulate the menstrual cycle, also relate to the incidence of vaginal yeast infections. These hormones do two primary things that help to stimulate yeast overgrowth: increase the amount of sugar in the vagina, and raise the pH of the vagina. To understand why your yeast infections occur at a specific time, we have articles dedicated to yeast infections that happen before, during, and after your period. We also have an article on yeast infections that occur during ovulation; and, a solid explanation for why your period may be late, or missed, due to Candida. We will talk about each of these sections in this article. If you have some time, you may want to check out the specific section that pertains to your situation!
Sugar, is of course, the food for yeast. Without food, the yeast couldn’t grow in the first place. And, when you provide yeast with food they will grow as quickly, and as fast, as they can. In some ways, they are a bit like gremlins. Consequently, your period really is associated with yeast infections, primarily because there are elevated levels of sugar in the vagina right before, and right after it.
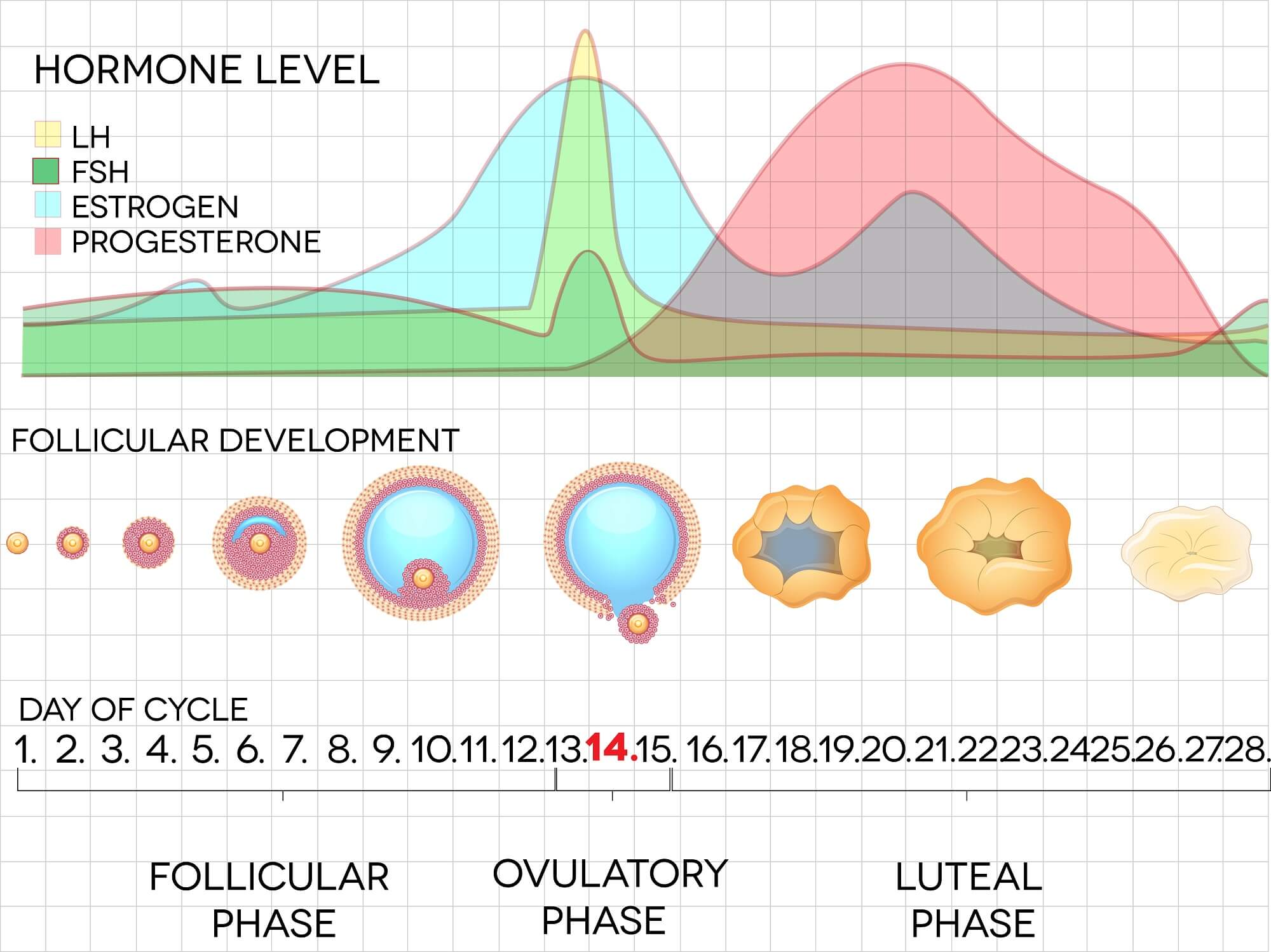
Vaginal pH is also altered during menses phases, and is consequently, related to Candida overgrowth. Menstrual cycle hormones are responsible for the alteration vaginal pH. Estrogen is inversely correlated with vaginal pH; i.e., the higher estrogen levels are, the lower pH will become. Follicle stimulating hormone; however, is directly correlated to pH levels; i.e., a higher level of follicle stimulating hormone will cause a higher pH. And, if you did not know, a low pH is acidic and a higher pH is alkaline.
Vaginal pH ideally needs to be acidic to keep Candida yeast from growing well. If your vaginal pH is too alkaline, this causes it to be more of an ideal environment for yeast to multiply in. A healthy vagina has a pH close to about 4 (water has a pH of 7). Consequently, you want an acidic vagina at all times—especially if you have a history of yeast infections. Using a tampon can greatly increase the pH of the vagina; as blood has a pH of about 7.35. So, when you use a tampon during your menstrual flow, you trap the fluid in the vagina; and, this “waters down” the vagina—raising the pH. When the pH becomes ideal of Candida growth, it can overgrow and start causing symptoms; thus, you seem to get a yeast infection during or after your period.
The chart below will show you a good approximation of the levels of these hormones at the various time frames of the menstrual cycle. Please note that estradiol is used in other types of charts, and is a main type of estrogen; hence, think of the estradiol level simply as estrogen. There is also a video that details the female reproductive cycle below; and, should also help you get acquainted with the hormones related to your period. We will then discuss what this then means, given this information.
A 1/2 Day & Yeast is Gone!
Linda Allen suffered from yeast infections for years. Through researching natural medicine & Candida, she found an efficacious solution!
Linda is one expert you want on your side! Let her show you how to get rid of a superficial yeast infection in just 12 hours; AND, keep it gone!
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Candidiasis & Menstruation Research
A study, published in Infection and Immunity [68.2 (2000): 651-657], found that estrogen, not progesterone, played a key role in allowing Candida to cause vaginal infection. The study was done on murine animals; and, various animals were given different hormones. The study found that estrogen given before inoculation, and after inoculation of Candida, caused the mice to get yeast infections. The study found that by inducing pseudo-estrus (giving mice hormones to simulate estrus; i.e., the period in mammals where they are sexually fertile) via administering estrogen, the Candida infections persisted much more. When estrogen levels were allowed to go back to normal, yeast infections had a hard time persisting. Increasing the estrogen levels beyond levels at estrus, did not cause more Candida development. So, normal physiological maximums of estrogen, appeared to be the most estrogen could influence Candida development. To speculate why this may be, the researchers also showed that vaginal outer (epithelial) cells also were less able to fight of Candida in the presence of estrogen; causing their to be an immune system correlation with estrogen levels.
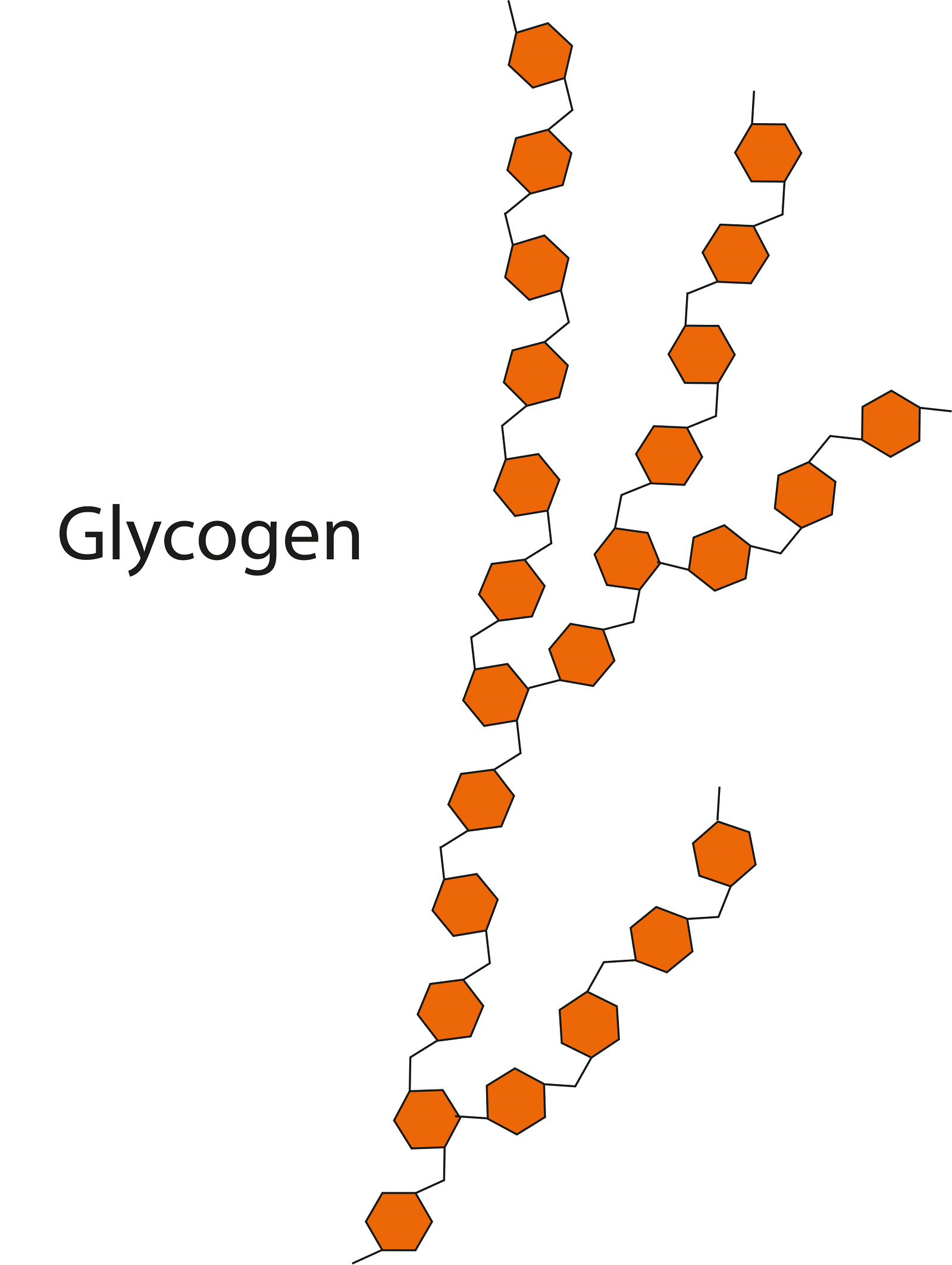
The way estrogen seemed to influence Candida development, and then peak at normal physiological maximum levels, is likely due to the vagina’s glycogen (a sugar) synthesis mechanism. The vagina can only take on so much glycogen; and, this process is regulated by estrogen. Thus, when estrogen is given above levels the body can make, the cells in the vagina are simply at their maximum capacity to synthesize glycogen; so, more estrogen cannot cause cells to become more “sugary.” Bitman, et al. (1965), found this maximum capacity for glycogen synthesis in rats; and, the rate of sugar creation could not be increased by adding estrogen beyond normal physiological peaks.
Since glycogen is a prime food for Candida, the presence of this sugar, is likely why Candida can thrive and start an infection. Also, as stated, a atrophied ability of vaginal epithelial cells to fight off Candida, no doubt also contributes to infection. The authors of the Infection and Immunity [68.2 (2000): 651-657] study, speculated that the peak of estrogen levels right before ovulation usually instigated a Candida infection; and, the higher steady levels of estrogen during the luteal phase, took the initial infection and allowed it to develop and become symptomatic. The study had this to say relating to such a hypothesis:
Based on these data in animals, estrogen is predicted to be the primary factor in the susceptibility to vaginitis during the luteal phase of the menstrual cycle, despite higher concentrations of progesterone than estrogen during that time. This is also consistent with the lack of prevalence of Candida vaginitis in women taking progesterone contraceptives. On the other hand, one may speculate that it is the peak levels of estrogen during the short ovulatory phase of the menstrual cycle that precipitate the vaginal infection and that the symptomatic infection does not fully present itself until the luteal phase.
http://dx.doi.org/10.1128/IAI.68.2.651-657.2000

Another research study, published in the Australasian Journal of Dermatology [53.4 (2012): 247-254], focused on chronic vaginal yeast infections and what medical science has learned up to that point. According to the study, vaginal yeast infections are often characterized by happening at a routine interval in the menstrual cycle. This is all due to the oscillating levels of estrogen in the body; due to a woman’s reproductive cycle. The majority of women report, that their yeast infection symptoms, are the worst after ovulation. This would be in line with what we just discussed (Candida gets a foothold right before ovulation and then is sustained after ovulation before menses; again, all due to glycogen synthesis). The peak of women’s reported symptom severity, happens in the premenstrual week; and, rapidly gets better during menstruation. Clinical symptoms often appear nonexistent after menstruation for a few days.
The study also stated that young girls, who have not had their period, and older postmenopausal women, rarely develop vaginal yeast infections. Also, Candida is also rarely found in a postmenopausal woman's vagina. This all changes when an older woman, past menopause, engages in estrogen hormone replacement therapy. Research was cited, that postmenopausal women not on estrogen therapy, had a rate of vaginal Candidiasis of 4%. Conversely, women on estrogen drugs, had a vaginal Candidiasis rate of 26%. Again, the study speculated the correlation of estrogen levels with yeast infections, was due to glycogen synthesis in the vagina—stimulated by this sex hormone.
What will Help?
Well, to help reduce the recurrent yeast infections, that seem to happen after ovulation, you can stop taking estrogen containing drugs; such as birth control pills. Some women may not make enough estrogen to max out their vagina’s glycogen synthesis; so normally, the sugar content of the vagina is lower. When estrogen is added to the body, there is plenty of capability of the cells to generate sugar, and the extra estrogen starts triggering the cells to make the most sugar they can. Thus, by reducing estrogen, you will also lower the amount of sugar in the vagina; and thus give yeast a harder time growing and causing symptoms to occur.
Another thing you can do, is make sure your vaginal probiotic bacteria are thriving. The primary genus of bacteria in a healthy female vagina is Lactobacillus. A healthy female’s vaginal fluid will have around 95% of the microorganisms comprised of Lactobacillus bacteria (Anukam, 2006). Many of the Lactobacillus bacteria, will eat up sugar; and also, some can create lactic acid—which will help to keep the vagina acidic and unconducive to Candida development. By adding a probiotic pill, containing live cultures of bacteria like L. acidophilus to the vagina for a few weeks, you will help to ensure there is less food, and the vagina stays in a healthy, acidic state.
Eliminate Bacterial Vaginosis & Vaginal Odor
Jennifer O’Brien is one prominent expert on BV that knows how to get rid of vaginal odor. BV is a common infection that you don’t have to put up with.
Jennifer will show you how to naturally eliminate vaginal odor in just 3 days.
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Yeast Infections Before Periods

Do you seem to get a yeast infection before your period? If you look at the menstrual cycle picture, showing hormone levels, you will see that progesterone is at a high level right before your menstrual flow begins. As estrogen causes the cells in the vagina to start taking on glycogen; right before your period, elevated levels of estrogen have caused the cells in your vagina to be rich in sugar.
You may have an aggravated form of Candida living in your vagina that has sent tendrils (known as hyphae) into your vaginal tissue. One study, published in Cellular and Molecular Life Sciences [October 1997, Volume 53, Issue 9, pp 744-749], determined that mycelial growth (tendril forming growth) of three Candida albicans species was profoundly augmented by the presence of estrogen. Another study, published in The Journal of Infectious Diseases [Volume 181, Issue 4, Pp. 1441-1446}, found that all three tested strains of Candida albicans grew more aggressively in the presence of estrogen. Thus the long duration, of slightly high estrogen levels before your period, may cause the yeast to grow aggressively; possibly sending tendrils into your vaginal tissue.
It is logical to assume, that the yeast is indeed growing into your tissue; because significant amounts of your vaginal tissue have not been shed—as it is before your period. Therefore, you may very well get a yeast infection, before menstruation and not after it, because the yeast is present deeper in your vaginal tissue—which is rich in sugar.
Candida Hub has a full article detailing the causes of a yeast infection before a period; and, several resources to start treating your condition naturally. Whatever type of infection you may have, you will probably be able to get a solution at Candida Hub. If you would like to learn more about this topic, you can always check this article out: Yeast Infection Before Period.
Clair Goodall: Author & Nature Lover
Clair Goodall is a bee-obsessed natural medicine convert from Minnesota. She is one expert you might want to know more about!
Clair will help you protect you and your family from toxic products and chemicals and help you discover solutions from nature.
Also, Clair’s book is backed by a 60-day, 100% money back guarantee
Visit Official Site!Yeast Infections After Periods
If you get a yeast infection right after your period, this is probably due to the excess sugars that are floating around your vagina and a lack of vaginal acidity. Remember, lower levels of estrogen raise the pH of the vagina; making it more conducive to yeast overgrowth. Progesterone is released to trigger the shedding of sugar rich vaginal cells—thus you have your menstrual flow. These cells may not fully be removed from the vagina after your period; providing extra food for yeast. And, as mentioned, a less acidic environment is probable; as estrogen levels are low after your period.
Consequently, it is likely that you could benefit from reducing the amount of sugar in your vagina and reducing the pH. Probiotics like L. acidophilus can do both of these things; and, it may be, that you could be greatly helped by enriching your vaginal microbiota (environment of microorganisms) with probiotics. If you’d like to learn more about probiotics, you can check this article out: Probiotic Yeast Infection Pills.
If you would like more information on Candida’s appearance after your period, you may find this article informative: Yeast Infection After Period.
Yeast Infection During Your Period
Do you seem to get yeast infections at the same time you have your period? As you recall, estrogen elevates the level of sugar in the vaginal cells before they are shed. Once progesterone triggers your menstrual flow, these cells begin to break away and fill the vagina. Thus, there is more available food for Candida to consume. To stop your yeast infections, you need to use a natural remedy to eliminate Candida from the vagina; and, use a good probiotic to help keep it gone. Standard protocol for yeast infection treatment.
Additionally, it may help to use water, or vinegar with water, to flush out the vagina during menses. Just make sure not to use too strong of a concentration of vinegar in the vagina; a 1% concentration should be sufficient. Strong concentrations of vinegar can cause irritation and chemical burns to occur so be careful (for more information about vinegar you can check out this article: Apple Cider Vinegar for Yeast Infection).
You may have heard it said, that douching is harmful to the vagina. This is, most likely, a spurious correlation touted as direct. The real cause of douching problems, is likely the harsh synthetic chemicals present in douche products. Cleaning out the vagina with water (avoid soap, as soap is quite alkaline) should really help mechanically remove yeast cells and the shed material Candida can use as food.
We have a whole article discussing why women get a yeast infection during their periods. If this sounds like something you’d like to know more about, you can peruse this article here: Yeast Infection During Period.
Yeast Infection During Ovulation
Do you tend to get yeast infections at the same time you’re ovulating? This may very well be because your vaginal pH is not properly balanced. The presence of estrogen helps to lower vaginal pH; and, at the time of ovulation, the estrogen level amount dips dramatically. Additionally, one study, published in the American Journal of Obstetrics and Gynecology [07/1997; 176(6):1270-5], proved that follicle stimulating hormone is directly correlated with pH; i.e., this hormone’s presence, raises pH. At the start of ovulation, follicle stimulating hormone spikes and estrogen levels fall. Thus, pH begins to rise during ovulation.
Because vaginal pH becomes much more conducive to Candida during ovulation, and this is when you seem to get infected, it is reasonable to conclude your problem is primarily pH related.
To effectively keep yourself from getting another yeast infection, you should look into using a probiotic packed with lactic acid producing bacteria. These bacteria will help to acidify your vagina, and keep it from being a "pH haven" for Candida. Again, we have a whole article devoted to this discussion. If you would like to learn a bit more about this topic, you may want to peruse this article: Yeast Infection During Ovulation.
A Natural, 12 Hour Yeast Infection Cure

According to a research paper published in Clinical Microbiology Reviews [12.1 (1999): 80-96], Candida species are quite ubiquitous organisms. Candida are most frequently present in the mouth; and, live in 31% to 55% of healthy people. The species that causes approximately 70% to 80% of all Candida infections is C. albicans.
The Chinese Journal of Obstetrics and Gynecology [2011 Jul;46(7):496] reports there appears to be a correlation between intestinal Candida infections and vaginal yeast infections. And, this provides a clue, as to why yeast infections in general, can reoccur.
This study states, in 148 cases of vaginal candida infections, 33.1% of the women were infected in both the intestines and vaginal area. The recurrence rate of yeast infections, in women with simultaneous intestinal infection, was significantly higher than for women who did not have an intestinal infection. This study concluded that vaginal yeast infections are highly associated with simultaneous intestinal Candida infection.
As research appears to indicate, systemic Candida infections can and do happen. A more systemic Candida infection may primarily get a foothold in the intestines; and cause a wide array of problems. If your yeast infections keep happening, a systemic Candida problem may be why.
One woman who suffered from a systemic Candida infection, for about 12 years, was Linda Allen. The systemic Candida infection that attacked Linda caused a wide range of health problems in addition to yeast infections. Some of these problems, Linda describes in her own words in the following quote:
To be honest, it was hard to pinpoint exactly what was wrong: I wasn’t really sick, but I wasn’t really well either. I had listlessness, fatigue, brain fog, stomach ailments, unexplained rashes, skin infections, and so on. It seemed like every day brought a new challenge.
My energy was sapped and I felt exhausted, which affected my grades and put a big dent in my social life.
Linda Allen’s symptoms included an embarrassing vaginal discharge, severe itching, and burning sensations. Her infections were difficult to deal with, and Linda’s health problems cost her financially as well. Linda states these infections of Candida can become excruciating when they happen as frequently as a menstrual period.
Yet, Linda spent a great deal of time in research; and even questioned health professionals who were kind enough to share some time with her. Linda even tried an array of purported "cures." Although it took a while, eventually, Linda put together a natural treatment plan she hoped would solve her Candida situation.
After spending about a year refining her new approach, Linda tried her system on herself. It worked amazingly well. Linda even returned to a few medical doctors to get tested for the presence of infections. These tests revealed all indicators of infection had vanished! Linda was indeed well again, after such a long, difficult journey.
Linda has since published a book detailing how to copy her success. She also includes a 12 hour yeast infection cure that can get rid of a superficial (such as a genital yeast infection or oral thrush) yeast infection in about 12 hours.
Linda’s publisher protects those who get her book with a 60 day, 100% money back guarantee. Linda’s publisher, a subsidiary of the United States based firm Keynetics Incorporated, is a reputable digital retailer that has been around for a long time. They have great customer service, and make getting a full refund on Linda’s book quick and easy. If you’re not satisfied, you can quickly get all your money back.
If you would like to learn more about Linda’s journey to freedom from Candida, see reviews of others who tried her natural system, or find out more about her efficacious book; you can find more information at Linda Allen’s website.
Author: Mr. Nicholas Gross

Nick Gross is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Nick is primarily a web developer but also researches and authors written and video content about natural health. Nick has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Affiliate Disclosure
Some of the links provided on this website are affiliate links. When a purchase is made through these links, Candida Hub earns money from commission. This helps to keep the website up and helpful to people for free. Thank you for any support!
Stay Up to Date
If you enjoyed this article, consider following / liking our Facebook page. This page is primarily utilized to alert followers of new articles that are put on Candida Hub. Candida related news is also discussed. While you are there, you can see what has been more recently added to Candida Hub.
SOURCES:
- http://dx.doi.org/10.1128/IAI.68.2.651-657.2000 — Fidel, Paul L., Jessica Cutright, and Chad Steele. "Effects of reproductive hormones on experimental vaginal candidiasis." Infection and immunity 68.2 (2000): 651-657. PubMed Full Text
- http://dx.doi.org/10.1210/endo-76-1-63 — BITMAN, JOEL, et al. "Kinetics of in vivo glycogen synthesis in the estrogen-stimulated rat uterus." Endocrinology 76.1 (1965): 63-69. PubMed
- http://dx.doi.org/10.1111/j.1440-0960.2011.00860.x — Fischer, Gayle. "Chronic vulvovaginal candidiasis: what we know and what we have yet to learn." Australasian Journal of Dermatology 53.4 (2012): 247-254. PubMed
- http://dx.doi.org/10.1097/01.olq.0000175367.15559.c4 - Anukam, Kingsley C., et al. "Lactobacillus vaginal microbiota of women attending a reproductive health care service in Benin city, Nigeria." Sexually transmitted diseases 33.1 (2006): 59-62. PDF Available Here, PubMed
- http://dx.doi.org/10.1016/j.micinf.2006.01.003 — Anukam, Kingsley, et al. "Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo controlled trial." Microbes and Infection 8.6 (2006): 1450-1454. PDF Available Here, PubMed
- http://www.ncbi.nlm.nih.gov/pubmed/9368671 — White, S., and B. Larsen. "Candida albicans morphogenesis is influenced by estrogen." Cellular and Molecular Life Sciences CMLS 53.9 (1997): 744-749.
- http://dx.doi.org/10.1086/315406 — Zhang, Xiaoqian, et al. "Estrogen effects on Candida albicans: a potential virulence-regulating mechanism." Journal of Infectious Diseases 181.4 (2000): 1441-1446. Full Text Available Here
- http://dx.doi.org/10.1016/S0002-9378(97)70345-4 — Caillouette, James C., et al. "Vaginal pH as a marker for bacterial pathogens and menopausal status." American journal of obstetrics and gynecology 176.6 (1997): 1270-1277.. PDF Available Here
- https://doi.org/10.1128/CMR.12.1.80 -- Fidel, Paul L., Jose A. Vazquez, and Jack D. Sobel. "Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans." Clinical Microbiology Reviews [12.1 (1999): 80-96].
- https://pubmed.ncbi.nlm.nih.gov/22041440/ -- Lin XL, Li Z, Zuo XL. "Study on the relationship between vaginal and intestinal candida in patients with vulvovaginal candidiasis." Chinese Journal of Obstetrics and Gynecology (Zhonghua fu chan ke za zhi). [2011 Jul;46(7):496].