See all "Menstruation" Section Topics

Yeast infections before your period, are typically caused by increased amounts of sugar in the vaginal tissue, or a lower pH. Estrogen levels were previously higher, right up until ovulation begins. Estrogen causes the cells in your vaginal wall to start enriching themselves with glycogen (a type of sugar). Thus, if yeast cells have invaded the inner lining of your vagina, through growing tendrils (hyphae), they will be able to find more sugar to feed upon.
Before you have your period, your body is secreting higher levels of the hormone progesterone. This hormone, signals to your body to start shedding some of the vaginal lining. It is possible that some amounts of tissue are shed, before you experience your period, due to the high amount of progesterone that is in the body. The tissue shed, will contain glycogen; providing food for Candida utilize for further development.
Vaginal pH also plays a role in helping a yeast infection to occur before your period. Estrogen levels drop shortly after the very beginning of ovulation, and right before menstruation. Estrogen levels are inversely related to vaginal pH (the more estrogen in a woman’s body, the lower pH her vagina will be at). According to a study published in Endocrinology [2005 Feb; 146(2): 816–824], estrogen causes the cells in the vagina to have acidic secretions.
Thus, it is likely, that yeast infections before a period, are due to a higher vaginal pH; and the greater availability of sugar in the vagina. If you have had recurrent vaginal Candidiasis, before your period, it is possible that the yeast have grown into your vaginal tissue. Because the yeast’s hyphae go into the vaginal lining, they are better able to feed on the glycogen estrogen has caused the cells to take on. Thus, each time your cells acquire more sugar before menstruation, yeast overgrows and you get an infection.
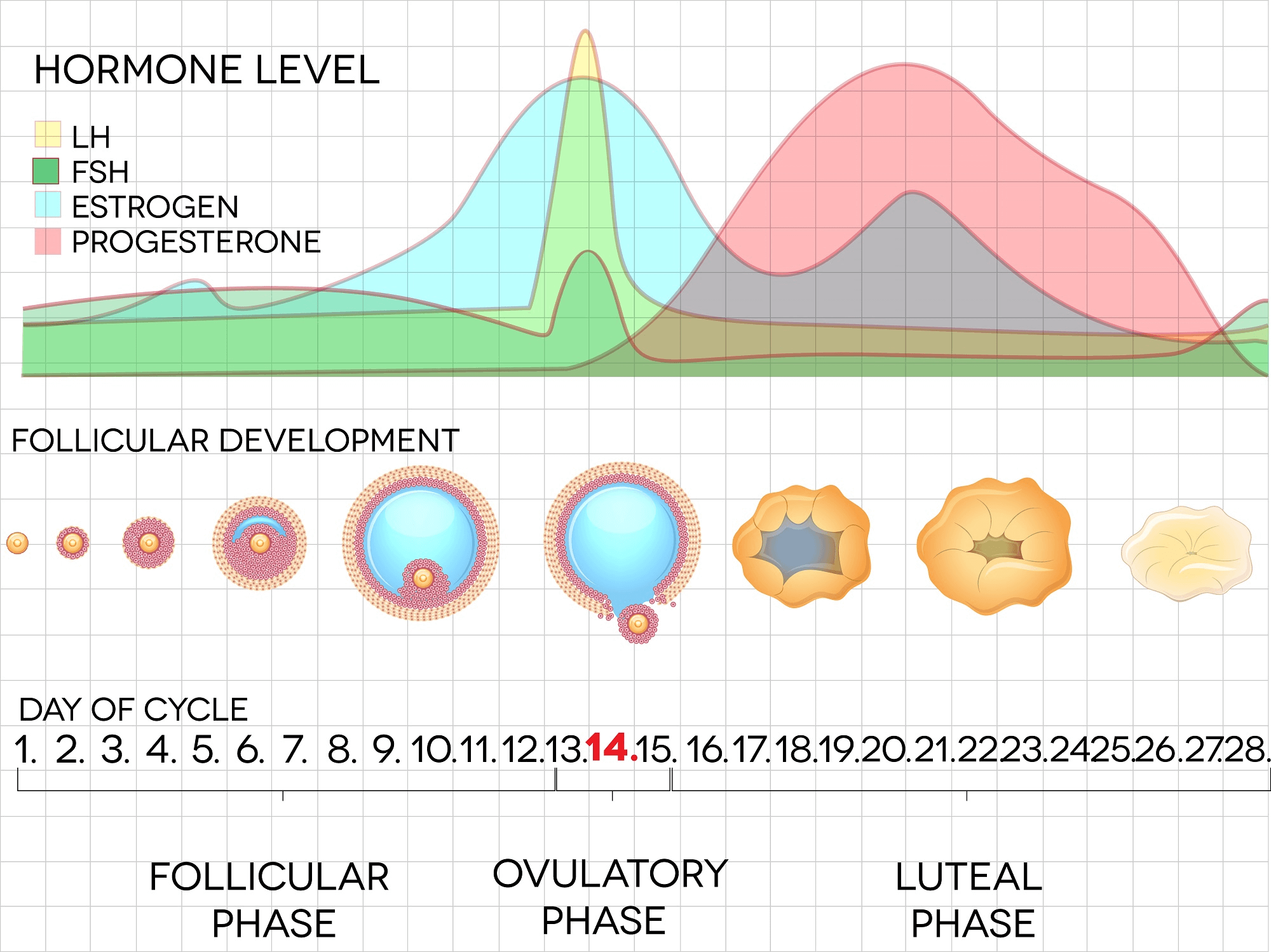
To better understand your hormone levels, during the menstrual cycle, the chart below is provided as a visual illustration.
A 1/2 Day & Yeast is Gone!
Linda Allen suffered from yeast infections for years. Through researching natural medicine & Candida, she found an efficacious solution!
Linda is one expert you want on your side! Let her show you how to get rid of a superficial yeast infection in just 12 hours; AND, keep it gone!
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Progesterone and the Immune System
Elevated glycogen, and higher pH, may not be the only reasons you are experiencing yeast infections before periods. As the above graph explains, progesterone is significantly elevated in the days prior to your period. Progesterone’s effects on the immune system, was documented by a study published in Microbiology and Immunology [Volume 39, Issue 6, pages 405–409, June 1995]. The study examined the reaction of white blood cells to progesterone; specifically, their ability to fight Candida. The study found that progesterone seemed to significantly hinder the ability of white blood cells to fight Candida in rats that also had been pretreated with estrogen.
If you are currently taking an estrogen birth control pill, this may play a critical role in your development of vaginal Candidiasis. The rats in the study were pretreated with estrogen, and given doses of progesterone. Similarly, your progesterone levels are elevated before your period—at the same time estrogen levels are naturally lower. If you have an elevated level of estrogen due to birth control pills, you are in a similar state the pretreated rats were in: a state of high estrogen and high progesterone. Consequently, the ability of your white blood cells to fight Candida, could be significantly weakened.
To prevent the weakening of your immune system, you may want to try taking a non-estrogen birth control pill; or, if you're taking a high dose estrogen pill, change to a low dose estrogen pill. The study found, that rats who did not have high levels of estrogen, had stronger immune response to Candida.
Additionally, elevated levels of estrogen in the body may also cause the vaginal lining to be over enriched with glycogen (a type of sugar).
Eliminate Bacterial Vaginosis & Vaginal Odor
Jennifer O’Brien is one prominent expert on BV that knows how to get rid of vaginal odor. BV is a common infection that you don’t have to put up with.
Jennifer will show you how to naturally eliminate vaginal odor in just 3 days.
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Lower Levels of Progesterone
A drop in both estrogen and progesterone, signals the body to shed the vaginal lining. If your body drops these levels too low before your period, you may have more sugar rich cells shed into the vagina. This may even be unoticable; as you do not have any vaginal discharge. Thus, yeast infections would be more likely.
One study, postulated that there was a link between lower levels of progesterone and increased vaginal Candidiasis. The study was published in the European Journal of Obstetrics & Gynecology and Reproductive Biology [Volume 131, Issue 2, April 2007, Pages 198–202]. The study looked at women after ovulation and before their menstruation; i.e., the luteal phase of the menstrual cycle. There were 50 women who participated in the study; and, 84 luteal phases of menstruation were analyzed. According to the study:
Significantly lower progesterone levels in the RVVC [recurrent vulvovaginal candidiasis] patients as compared to the healthy controls suggest a link between an altered hormonal status and one of possible causes of RVVC in these women.
http://dx.doi.org/10.1016/j.ejogrb.2006.03.009
Clair Goodall: Author & Nature Lover
Clair Goodall is a bee-obsessed natural medicine convert from Minnesota. She is one expert you might want to know more about!
Clair will help you protect you and your family from toxic products and chemicals and help you discover solutions from nature.
Also, Clair’s book is backed by a 60-day, 100% money back guarantee
Visit Official Site!How Estrogen Relates to Candidiasis
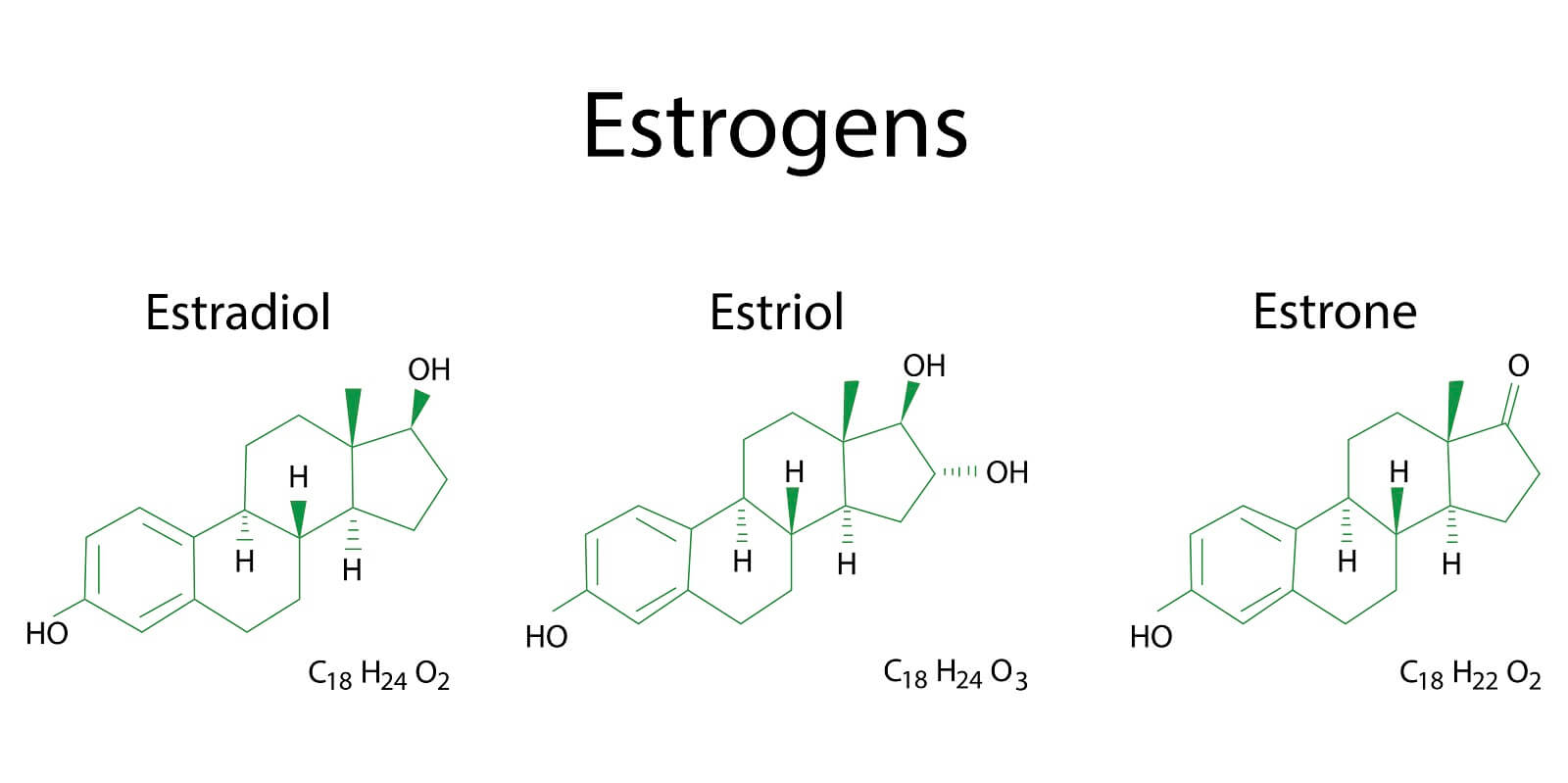
Vaginal Candidiasis usually revolves around the changing levels of estrogen in the body. The primary reason estrogen correlates so strongly with vaginal Candidiasis, is that this sex hormone directly causes vaginal cells to synthesize the sugar glycogen. As estrogen levels rise, these cells create more and more sugar. This sugar is a wonderful food for Candida to start devouring; and, it does consume it. The result is a rapid progression towards infection. The majority of women, who see menstrual phase occurrences of yeast infections, report that their symptoms get worse after they ovulate. Right before ovulation, estrogen peaks sharply. This short time of accelerated glycogen synthesis, can be the initiation of Candida overgrowth. As time progress, and a woman enters the luteal phase of her menstrual cycle, estrogen climbs again and remains steady. Thus, the yeast, that got a foothold before ovulation, begins to multiply and sustain its growth. Thus, the week right before your period, you may notice the worst yeast infection symptoms; as this may be the height of Candida’s development.
A study discussing this correlation between estrogen and yeast infections before a period, was published in the Australasian Journal of Dermatology [53.4 (2012): 247-254]. The study stated, that most women have the worst symptoms after ovulation—particularly the week right before menstruation. The study states that after estrogen levels drop during menstruation, many clinical signs of a yeast infection can disappear; often being totally gone up to a few days after menstruation.
The study also cited research that shows women rarely get vaginal yeast infections after menopause. The exception, is that such infections occur almost completely in women who are on some type of estrogen replacement therapy. This study demonstrated the importance of estrogen in the causation of vaginal candidiasis. The research study also seemed to speculate, that because women who get vaginal yeast infection rarely develop oral infections, this could be a result of estrogen hindering the vaginal immune system. This is possibly due to the abundance of estrogen receptors in the vaginal tissue.
Another study, published in Clinical and Experimental Immunology [33.1 (1978): 79], also looked at the affects of progesterone and estrogen (estradiol) on Candida albicans prevalence. The study used women with normal hormonal patterns, males, women on a oral contraceptive, and women who had gonadal dysgenesis (a dysfunction of the gonads that results in much less, or no sex hormone production). The study found that Candida albicans was much more prevalent in women in the luteal phase than women in the follicular phase. Women with gonadal dysgenesis, had Candida levels comparable to males; but, they were much lower than women in the follicular phase of the menstrual cycle. Those women, who took an estrogen containing birth control pill, had more Candida overgrowth.
Probiotic Supplements
In addition to killing off the yeast with natural remedies, you would do well to start taking a probiotic to help keep yeast away. It is a great idea to take a probiotic supplement orally, and to insert it into the vagina as well. This will help your gut maintain good health inducing microbiota; and, your vagina will be much more resistant to future outbreaks of Candida.
A Natural, 12 Hour Yeast Infection Cure

According to a research paper published in Clinical Microbiology Reviews [12.1 (1999): 80-96], Candida species are quite ubiquitous organisms. Candida are most frequently present in the mouth; and, live in 31% to 55% of healthy people. The species that causes approximately 70% to 80% of all Candida infections is C. albicans.
The Chinese Journal of Obstetrics and Gynecology [2011 Jul;46(7):496] reports there appears to be a correlation between intestinal Candida infections and vaginal yeast infections. And, this provides a clue, as to why yeast infections in general, can reoccur.
This study states, in 148 cases of vaginal candida infections, 33.1% of the women were infected in both the intestines and vaginal area. The recurrence rate of yeast infections, in women with simultaneous intestinal infection, was significantly higher than for women who did not have an intestinal infection. This study concluded that vaginal yeast infections are highly associated with simultaneous intestinal Candida infection.
As research appears to indicate, systemic Candida infections can and do happen. A more systemic Candida infection may primarily get a foothold in the intestines; and cause a wide array of problems. If your yeast infections keep happening, a systemic Candida problem may be why.
One woman who suffered from a systemic Candida infection, for about 12 years, was Linda Allen. The systemic Candida infection that attacked Linda caused a wide range of health problems in addition to yeast infections. Some of these problems, Linda describes in her own words in the following quote:
To be honest, it was hard to pinpoint exactly what was wrong: I wasn’t really sick, but I wasn’t really well either. I had listlessness, fatigue, brain fog, stomach ailments, unexplained rashes, skin infections, and so on. It seemed like every day brought a new challenge.
My energy was sapped and I felt exhausted, which affected my grades and put a big dent in my social life.
Linda Allen’s symptoms included an embarrassing vaginal discharge, severe itching, and burning sensations. Her infections were difficult to deal with, and Linda’s health problems cost her financially as well. Linda states these infections of Candida can become excruciating when they happen as frequently as a menstrual period.
Yet, Linda spent a great deal of time in research; and even questioned health professionals who were kind enough to share some time with her. Linda even tried an array of purported "cures." Although it took a while, eventually, Linda put together a natural treatment plan she hoped would solve her Candida situation.
After spending about a year refining her new approach, Linda tried her system on herself. It worked amazingly well. Linda even returned to a few medical doctors to get tested for the presence of infections. These tests revealed all indicators of infection had vanished! Linda was indeed well again, after such a long, difficult journey.
Linda has since published a book detailing how to copy her success. She also includes a 12 hour yeast infection cure that can get rid of a superficial (such as a genital yeast infection or oral thrush) yeast infection in about 12 hours.
Linda’s publisher protects those who get her book with a 60 day, 100% money back guarantee. Linda’s publisher, a subsidiary of the United States based firm Keynetics Incorporated, is a reputable digital retailer that has been around for a long time. They have great customer service, and make getting a full refund on Linda’s book quick and easy. If you’re not satisfied, you can quickly get all your money back.
If you would like to learn more about Linda’s journey to freedom from Candida, see reviews of others who tried her natural system, or find out more about her efficacious book; you can find more information at Linda Allen’s website.
Author: Mr. Nicholas Gross

Nick Gross is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Nick is primarily a web developer but also researches and authors written and video content about natural health. Nick has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Affiliate Disclosure
Some of the links provided on this website are affiliate links. When a purchase is made through these links, Candida Hub earns money from commission. This helps to keep the website up and helpful to people for free. Thank you for any support!
Stay Up to Date
If you enjoyed this article, consider following / liking our Facebook page. This page is primarily utilized to alert followers of new articles that are put on Candida Hub. Candida related news is also discussed. While you are there, you can see what has been more recently added to Candida Hub.
SOURCES:
- http://dx.doi.org/10.1210%2Fen.2004-1153 — Estrogen Acidifies Vaginal pH by Up-Regulation of Proton Secretion via the Apical Membrane of Vaginal-Ectocervical Epithelial Cells. Endocrinology [2005 Feb; 146(2): 816–824]
- http://dx.doi.org/10.1111/j.1348-0421.1995.tb02220.x — Suppression of Anti-Candida Activity of Murine Neutrophils by Progesterone In Vitro: A Possible Mechanism in Pregnant Women's Vulnerability to Vaginal Candidiasis. Microbiology and Immunology (Volume 39, Issue 6, pages 405–409, June 1995). PDF Available here
- http://dx.doi.org/10.1016/j.ejogrb.2006.03.009 — Clinical aspects and luteal phase assessment in patients with recurrent vulvovaginal candidiasis. European Journal of Obstetrics & Gynecology and Reproductive Biology (Volume 131, Issue 2, April 2007, Pages 198–202)
- http://dx.doi.org/10.1016/j.jep.2012.01.045 — Biofilm inhibition by Cymbopogon citratus and Syzygium aromaticum essential oils in the strains of Candida albicans. Journal of Ethnopharmacology (Volume 140, Issue 2, 27 March 2012, Pages 416–423)
- http://dx.doi.org/10.1111/j.1440-0960.2011.00860.x — Fischer, Gayle. "Chronic vulvovaginal candidiasis: what we know and what we have yet to learn." Australasian Journal of Dermatology 53.4 (2012): 247-254. PubMed
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1537510/ — Mathur, S., et al. "Sex steroid hormones and antibodies to Candida albicans." Clinical and experimental immunology 33.1 (1978): 79. PubMed PDF
- https://doi.org/10.1128/CMR.12.1.80 -- Fidel, Paul L., Jose A. Vazquez, and Jack D. Sobel. "Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans." Clinical Microbiology Reviews [12.1 (1999): 80-96].
- https://pubmed.ncbi.nlm.nih.gov/22041440/ -- Lin XL, Li Z, Zuo XL. "Study on the relationship between vaginal and intestinal candida in patients with vulvovaginal candidiasis." Chinese Journal of Obstetrics and Gynecology (Zhonghua fu chan ke za zhi). [2011 Jul;46(7):496].