See all "Mucus" Section Topics

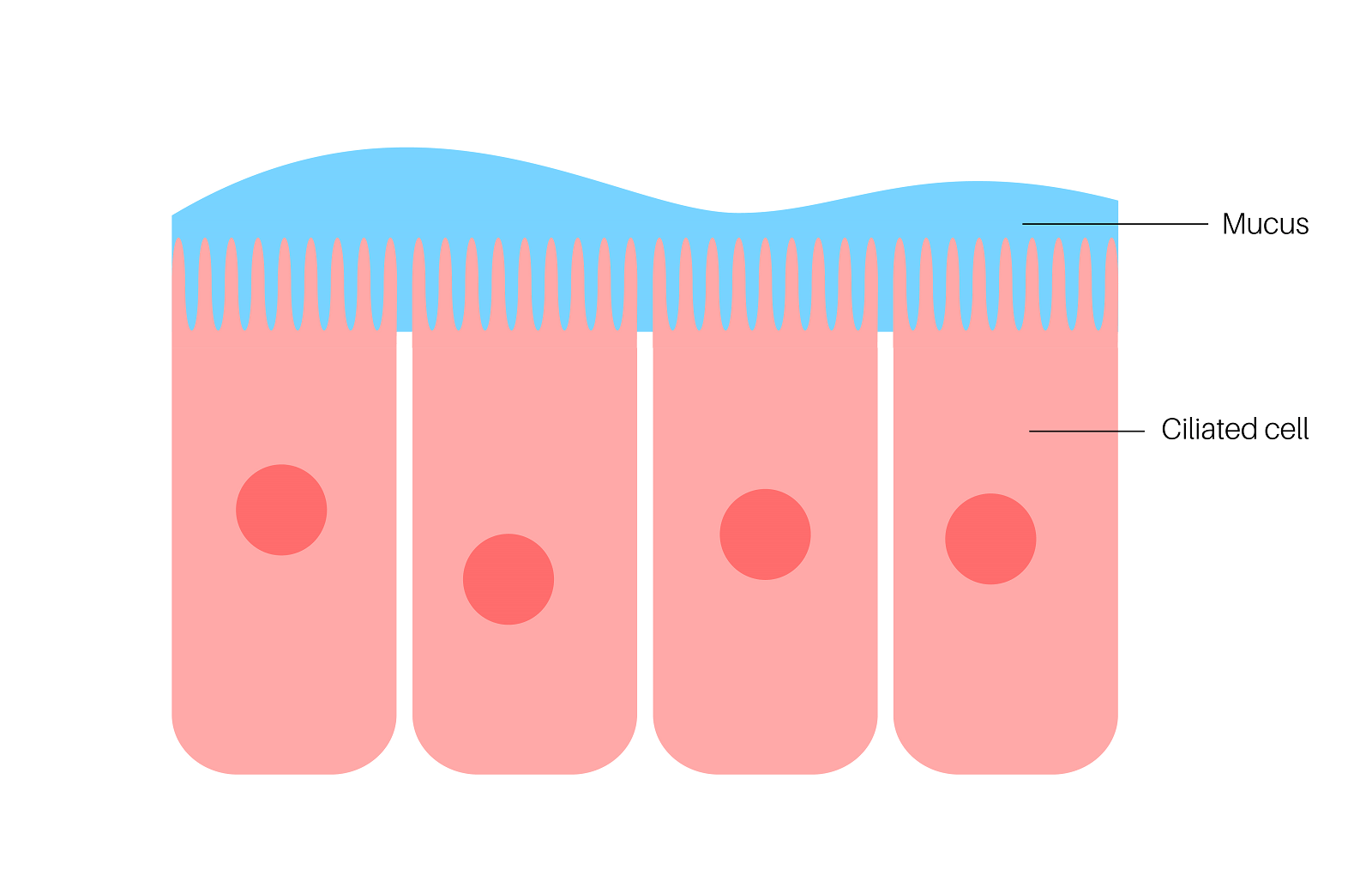
Cervical mucus is similar to other types of mucus the body synthesizes. If you are suspecting you have a yeast infection, and you see the yeast in your cervical mucus, this may be the case. The primary role of cervical mucus is to be a physical and chemical barrier to harmful pathogens. One way the cervical mucus does this is by entrapping pathogens, so that they can be more easily swept out of the vagina. It may be that your body is doing a good job of fighting a yeast infection if you notice yeast in your cervical mucus; as this means some of the yeast is being mechanically cleared away.
The primary component of mucus are the glycoproteins known as mucins. Mucins are protein chains that have carbohydrate molecules attached to them. Bacterial and fungal pathogens can attach to the carbohydrate chains on mucin; then becoming trapped in the mucus. After a pathogen like Candida latches on to a mucin, it stands much less of a chance of finding a place on the body to attach to; and, thus, is often swept away without doing harm. There are even symbiotic bacteria that live in mucus and help keep the body healthy.
When there is enough Candida growing in the vagina, it can sometimes lead to a vaginal discharge with the consistency of cottage cheese. Candida cells are dimorphic; meaning they can exist in two different physiological forms. One form is a round cell, known as a blastoconidia. The other form is a long germ tube, known as a hypha. As Candida develops, it can form networks of germ tubes, biofilm, and single blastoconidia cells. This sludge can occasionally build up to the point where it resembles a thick cottage cheese like substance. Your cervical mucus can push this cottage cheese like Candida build up out of your vagina; making it look like there is a cottage cheese like substance in your cervical mucus.
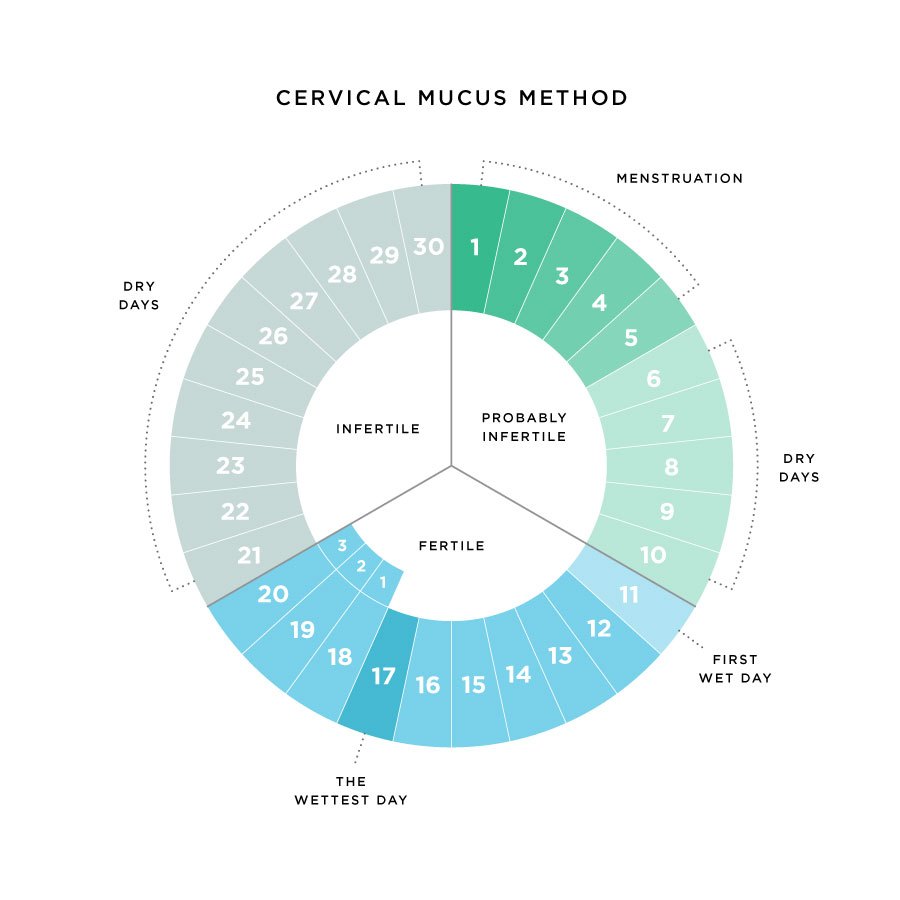
The presence of an infection may also spur on mucus production. If you are noticing more cervical mucus than usual, it could be you have an infection of the cervix of some kind. However, there are other factors, such as hormones, that affect the production of cervical mucus; so it is hard to say if an increase of this mucus is due to an infection. It could be that you are in the ovulatory phase of the menstrual cycle; at this time your cervical mucus is more hydrated. Thus, you may notice a discharge of mucus at this time.
A cottage cheese like discharge is a solid indicator of a yeast infection. If you do not have this, but are concerned you may have a vaginal Candida infection, you should consider other symptoms that present with this infection to get a correct diagnosis. Research has indicated that women who have had a yeast infection in the past are better at diagnosing one (Abbott, Jean; 1995). Yet, it is very difficult, even for medical professionals, to diagnose a yeast infection correctly; as so many other vaginal infections share similar characteristics. The article on cottage cheese vaginal discharge will explain what this particular symptoms means in more detail.
The main article for this section on Candida Hub, Yeast Infection & Excess Mucus, may also help answer some of your questions regarding Candida in your mucus.
At the close of this topical delineation, some natural therapies (an herb and two essential oils) will be discussed. These natural medicines may all have capable expectorant ability; in addition they are capable antifungals that stop Candida. Using these herbal therapies might help expel cervical mucus with Candida in it, from the body. Also, these natural therapies can help to mitigate an active yeast infection.
A 1/2 Day & Yeast is Gone!
Linda Allen suffered from yeast infections for years. Through researching natural medicine & Candida, she found an efficacious solution!
Linda is one expert you want on your side! Let her show you how to get rid of a superficial yeast infection in just 12 hours; AND, keep it gone!
A 60-day, 100% money back guarantee is provided.
Visit Official Site!What is Cervical Mucus?
A study, published in Acta Obstetricia et Gynecologica Scandinavica [47.sup1 (1968): 57-79], discusses the structure of cervical mucus. The study relates that cervical mucus can be considered a biological system consisting of 90% to 99% liquid, with constituents similar to saline (a mixture of some salt and water). The mucus also contains gel-forming mucoproteins, substances as colloidal solutions (colloids undergo brownian motion; therefore their particles do not settle; e.g., milk), and proteins. These components in the cervical mucus liquid can vary from comprising 11% of the solution, down to just 1.5%. The cervical mucus will have the most liquid in it during the middle of the menstrual cycle.
This study states cervical mucus is contributed to by the peritoneum, vagina, cervix, corpus, fallopian tubes, and ovaries. Concerning the changes in cervical mucus, mucoproteins are responsible for this.
Another study also discusses cervical mucus; this research was published in the Biophysical Journal [81.4 (2001): 1930-1937]. The study states the common fact that mucus is quite ubiquitous in the human body; covering the surface of the respiratory, reproductive, and gastrointestinal tracts. This outer covering of mucus provides a line of defense against pathogenic microbes.
The reason mucus is a gel-like substance is due to the mucins (which are categorized as mucoproteins) within it. Mucins are glycoproteins which have long strands of proteins with chains of sugars attached to them. The mucin strands sometimes interact with each other by attaching together. The mucins are highly glycosylated (they have a lot of sugar attached to the proteins); and, can be comprised of 80% sugar (carbohydrates) by weight. These mucins are entangled, and form a viscous, elastic gel.
Additional research we will discuss, relating to the composition of mucus, was published in the Proceedings of the National Academy of Sciences [110.26 (2013): 10771-10776]. The study states that mucus is a primary form of defense the body has against the outside world. The mucus layer is thoroughly colonized by bacteria; which include some symbiotic species. These symbiotic (or "probiotic") bacteria help via secreting antibiotic chemicals, providing nutrients, and bioluminescence.
The primary large molecules in the mucus are the mucins. Mucins have hundreds of branched chains of sugars that extend from the protein core. The human body uses a variety of methods to help limit the colonization of microbes in the mucus. When a pathogen invades a mucus membrane (an outer layer of tissue that secretes mucus), the response can be an increased secretion of mucus, production of antimicrobial chemicals, or an change of the composition of the sugar chains attached to the mucin protein backbone. By altering the carbohydrate structures attached to the mucin protein backbone, this can make the mucin more likely to attract a pathogen. Once a pathogen attaches to one of the sugar molecules on the mucin, it can become entrapped; then, easily cleared away as the mucin is shed.
Concerning the characteristics of cervical mucus mucins, a study discusses this topic; which was published in the Biochemical Journal [211.1 (1983): 13-22]. According to the research, cervical mucus carries out a vital role in the defense of the uterine cavity. Cervical mucus also controls spermatozoal migration and survival. The study relates that the amount of this mucus, and its physical properties, will change to some extent during the menstrual cycle.
During ovulation, estrogen secretion causes the cervical mucus to take on more water; resulting in a watery mucus with low viscosity and elasticity. After ovulation, in the last phase of the menstrual cycle (luteal phase), progesterone levels are high. In the luteal phase there is much less cervical mucus produced, and the mucus is more thick.
During pregnancy, a large mucus plug will cover the cervical canal. This mucus during pregnancy is more like the mucus produced in the luteal phase of the menstrual cycle. So, as you can tell, a woman’s cervical mucus should go through noticable changes as she progresses through the menstrual cycle, or enters pregnancy.
Concerning the mucins of the cervical mucus; as with other mucus; these provide the structural component of the mucus gel. The study was able to ascertain the composition of the mucins in cervical mucus. According to the research approximately 65% of the weight of these mucins is comprised of carbohydrates. Approximately 20% of the mucin weight is comprised of protein. Galactose was the major neutral sugar found in the molecules; glucose and mannose were present in trace amounts. Mucins can often have about 80% of their weight from carbohydrates; so we see that cervical mucus will have less sugar in it than, possibly, mucus from the respiratory system.
Eliminate Bacterial Vaginosis & Vaginal Odor
Jennifer O’Brien is one prominent expert on BV that knows how to get rid of vaginal odor. BV is a common infection that you don’t have to put up with.
Jennifer will show you how to naturally eliminate vaginal odor in just 3 days.
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Cervical Mucus & Candida
A study, published in the Glycoconjugate Journal [26.9 (2009): 1125-1134], looked at how the mucins in cervical mucus responded to Candida albicans. The study relates that cervical mucins are glycosylated proteins (proteins with sugars attached to them) that form the protective cervical mucus layer. To better understand how the sugar components of the mucin interacted with C. albicans, these carbohydrates were analyzed.
The study stated that approximately 20% of humans have a genetic trait that changes mucus membrane gland cells. This genetic trait causes there to be a loss of a type of fucose sugars in the gland secretions. This impaired fucosylation (the ability to add fucose sugars to a molecule) of the mucosal secretions in people with this genetic anomaly, causes a 2.4 to 4.4 times increase in the risk for having recurrent vaginal yeast infections by C. albicans. This risk, in women who have this genetic anomaly, is estimated to be 67% of the total risk for developing recurrent vaginal yeast infections.
The study states that sugars that contain fucose, in the mucus secretions, have been shown to be involved in interactions between pathogens and epithelial cells (cells lining the outside of a body surface, such as the interior lining of the stomach). Concerning C. albicans, the germ tubes of this fungal pathogen, have been shown to have the ability to specifically adhere to fucose.
The research also states that cervical mucus changes during the menstrual cycle, and that there is a relationship in this change to pathogen infection. This relationship is complex; as the cervical mucus provides not only a physical barrier to infection, but a chemical one as well. And, a lack of a chemical or physical impediment to infection offered by mucus, may present an opportunity for microbes to colonize and grow.
The study states that C. albicans infection can be more common in the luteal phase of the menstrual cycle, when using antibiotics, if a person has uncontrolled diabetes, using oral contraceptives, or when a person is undergoing hormone therapy. Because of this, it is possible that one class of cervical secretions allow for the growth and development of Candida, while another affects Candida cells adhesion (and thus their ability to colonize an area after they have attached).
The study stated it was possible for some mucins and other cervical secretion components to bind onto C. albicans. A major mucin produced by the cervix, fucosylated MUC5B, might bind to C. albicans; limiting the ability of the yeast cells to bind (attach) to vaginal cells. Also, shed vaginal epithelial cells in the mucus may also bind onto C. albicans, trapping them; thus, facilitating their removal from the vagina.
This research shows that C. albicans can attach to cervical mucus; and, shed vaginal cells in the mucus may also bind to C. albicans. This binding action helps to prevent the Candida cells from attaching to the body, and allows them to be carried out of the body. And, if you have a genetic anomaly, where you do not have enough fucose in your cervical mucus, this could put you at a much greater risk for developing recurrent vaginal yeast infections.
Clair Goodall: Author & Nature Lover
Clair Goodall is a bee-obsessed natural medicine convert from Minnesota. She is one expert you might want to know more about!
Clair will help you protect you and your family from toxic products and chemicals and help you discover solutions from nature.
Also, Clair’s book is backed by a 60-day, 100% money back guarantee
Visit Official Site!Getting Rid of Candida Colonized Cervical Mucus

Dr. Richard Marrs, in his book Dr. Richard Marrs’ Fertility Book, states that some types of fertility treatment can bring about too much cervical mucus. In cases where there is too much cervical mucus; or the mucus is too thick, this physician offers an interesting solution. Dr. Marrs directs women to take one tablespoon of an expectorant cough medicine every four hours starting two days before ovulation. Dr. Marrs says that in some cases, these expectorant cough medicines will thin the cervical mucus in the same way it thins the mucus in the lungs. Although this suggestion is for women hoping to improve fertility, it can be used to help remove cervical mucus that has Candida in it.
It is clear that cough medicine will not help in curing Candida in itself; yet, it can help get rid of such an infection merely by aiding in the removal of cervical mucus. What may work just as well, is using herbs or essential oils that are expectorants; and, in addition, also are also antifungals.
One herb that is an expectorant, and is a capable Candida fighter, is licorice root (Glycyrrhiza glabra). This herb contains glycyrrhizin and glycyrrhizic acid; which are anti-inflammatory. However, both of these chemicals can counteract the effects of estrogen, possibly making your cervical mucus less hydrated. Thus, because estrogen levels are at their lowest at the end and start of the menstrual cycle; you may want to avoid licorice at this time. However, due to the extra Candida fighting ability of licorice, it should probably not be ruled out at other times in your menstrual cycle. Having tea made from licorice root will help stop Candida; and, its expectorant ability may assist cervical mucus leaving the vagina—despite possibly being less hydrated.
The first essential oils that may assist in the removal of cervical mucus is lavender essential oil. Jennifer Rhind, in her book Fragrance and Wellbeing, states that French lavender (Lavendula stoechas) has folk medicinal uses; one of which is as an expectorant. Regular lavender oil (Lavandula angustifolia) may work just as well as an expectorant. Although possibly not the greatest essential oil to use for removing mucus; lavender oil is a decent Candida fighting oil. Therefore, you are really getting a good natural therapy for Candida while you help the body shed excess cervical mucus. A caution is lavender may be a uterine stimulant, causing the uterus to contract. You should try and avoid lavender oil if you are pregnant.
The next essential oil you can use as an expectorant and Candida fighter is thyme essential oil. Thyme oil is a very powerful Candida fighter. It is one of the best ways to naturally treat a yeast infection as a result. And, thyme oil is a known expectorant; which may help the body remove excess cervical mucus.
You may wish to put 2 drops of each essential oil in a tea made from licorice root. It may be safe to add more essential oil; however, be careful. Essential oils are very powerful substances. Be sure to follow the safety guidelines for each oil if you plan on ingesting more. Also, it may be wise to solicit the advice of a natural medicine professional before you give any essential oils internally to children.
An All-Natural, 12 Hour Candida Cure

Many people end up suffering from recurrent yeast infections, and most of them are women. In addition to yeast infections, when Candida has invaded a person’s body enough, it can cause a great deal of health problems. One woman who suffered from a systemic yeast infection was Linda Allen. Linda spent about 12 years of her life suffering from terrible, seemingly inexplicable, health complications. In addition to her poor health, she would get yeast infections.
Linda’s problems began in her teen years; after Linda went through a sinus infection she came down with a yeast infection. Linda sought the advice of a doctor for this problem, and she was prescribed an antifungal. The antifungal drug worked well, and soon Linda’s yeast infection cleared up. However, after some time had passed, Linda came down with another yeast infection. This type of problem would start to characterize her life.
Linda spent a small fortune on medical bills as she went through this struggle. At a time when she should have been able to afford a house to live in, Linda found herself living in a small apartment. The doctors simply did not provide a permanent solution to her health problems; they just were costing her a great deal of time and money. This situation, fortunately, changed when Linda visited a naturopath.
The naturopath Linda consulted knew exactly what her problem was: systemic Candidiasis. Although the naturopath did not provide a permanent solution to her problems, Linda was able to start her efforts to find a solution herself. Linda would end up spending a great amount of time researching Candida, and would try many different therapies herself.
Eventually, Linda’s hard work yielded a novel treatment plan. Once Linda developed her system, she spent about a year refining it; then, she tried it on herself. Linda found that her yeast infections went away using her new natural system. And, as time progressed, her systemic Candida cleared up. After so many years, Linda was finally in good health again.
Linda at first shared her discovery with others she knew were facing the same health issues with Candida she had been. When they tried her system, they too would recover and stay free from Candida. It wasn’t long before Linda published a book detailing her natural protocol for curing, not only yeast infections, but systemic yeast problems as well. Linda even explains how to naturally cure a yeast infection in 12 hours of time; and, keep it gone for good.
Linda has published her book with a large online publisher; a subsidiary of Keynetics Incorporated—a firm based in Boise, Idaho; USA. You can download Linda’s book online, making it easy to get started right away. Linda publisher offers a generous 60 day, 100% money back guarantee on Linda’s book. If you decide to try Linda’s book, and you find it unsatisfactory, you have a full 60 days to get a total refund. This guarantee can help; especially if you have tried other purported remedies for Candida that just did not work.
To find out more about Linda’s personal story, or to find out more about her book, you can get more information at Linda Allen’s website.
Author: Mr. Nicholas Gross

Nick Gross is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Nick is primarily a web developer but also researches and authors written and video content about natural health. Nick has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Affiliate Disclosure
Some of the links provided on this website are affiliate links. When a purchase is made through these links, Candida Hub earns money from commission. This helps to keep the website up and helpful to people for free. Thank you for any support!
Stay Up to Date
If you enjoyed this article, consider following / liking our Facebook page. This page is primarily utilized to alert followers of new articles that are put on Candida Hub. Candida related news is also discussed. While you are there, you can see what has been more recently added to Candida Hub.
SOURCES:
- http://dx.doi.org/10.1016/S0196-0644(95)70168-0 — Abbott, Jean. "Clinical and microscopic diagnosis of vaginal yeast infection: a prospective analysis." Annals of emergency medicine 25.5 (1995): 587-591.
- https://doi.org/10.3109/00016346809156845 — Odeblad, Erik. "The functional structure of human cervical mucus." Acta Obstetricia et Gynecologica Scandinavica [47.sup1 (1968): 57-79].
- https://doi.org/10.1016/S0006-3495(01)75844-4 — Olmsted, Stuart S., et al. "Diffusion of macromolecules and virus-like particles in human cervical mucus." Biophysical Journal [81.4 (2001): 1930-1937].
- https://doi.org/10.1073/pnas.1305923110 — Barr, Jeremy J., et al. "Bacteriophage adhering to mucus provide a non–host-derived immunity." Proceedings of the National Academy of Sciences [110.26 (2013): 10771-10776].
- https://doi.org/10.1042/bj2110013 — Carlstedt, I., et al. "Isolation and characterization of human cervical-mucus glycoproteins." Biochemical Journal [211.1 (1983): 13-22].
- https://dx.doi.org/10.1007/s10719-009-9234-0 — Domino, Steven E., et al. "Cervical mucins carry α (1, 2) fucosylated glycans that partly protect from experimental vaginal candidiasis." Glycoconjugate Journal [26.9 (2009): 1125-1134]. PubMed Full Text
- Google Books — Marrs, Richard. “Dr. Richard Marrs' Fertility Book: America's Leading Infertility Expert Tells You Everything You Need to Know About Getting Pregnant.” Random House Publishing Group [2011]. ISBN: 0307789470, 9780307789471
- Google Books — Rhind, Jennifer Peace. “Fragrance and Wellbeing: Plant Aromatics and Their Influence on the Psyche.” Singing Dragon [2013]. ISBN: 0857010735, 9780857010735