See all "Breasts" Section Topics

A yeast infection of the nipple can cause sharp shooting pain in the breast, and general burning pain in the nipple. If you are having anything like this, you might have Candida (the genus of fungi that causes yeast infections) infecting your nipple and areola skin. However, as research indicates, most women who have nipple pain do not usually have a problem with Candida. For breastfeeding women, improper feeding technique is a big reason why women can get sore, irritated nipples. In this article, we will discuss what symptoms to look for that indicate your nipple pain is related to Candidiasis. Also, the predisposing factors, that put you at greater risk for a yeast infection of the nipple, will be investigated. If you find that you have some predisposing factors for this condition, and you are exhibiting the classic signs of nipple Candidiasis; your problem may be due to yeast.
Also, we will discuss a quick, natural solution to get rid of a nipple yeast infection, as well. There are several other pages linked to in this section; and, if you have time, it might be helpful to read up on these natural remedies. If your baby is positive for oral thrush, it is even more likely that your nipples also have thrush. Take your baby to a pediatrician and get professional help for this problem. Many natural remedies are not suitable to use on such small infants, so avoid doing anything with your baby regarding natural medicine without first consulting a medical professional!
A 1/2 Day & Yeast is Gone!
Linda Allen suffered from yeast infections for years. Through researching natural medicine & Candida, she found an efficacious solution!
Linda is one expert you want on your side! Let her show you how to get rid of a superficial yeast infection in just 12 hours; AND, keep it gone!
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Diagnosing Nipple Yeast Infections

A study, published in BMJ Open [3.3 (2013)], sought to understand what symptoms were commonly associated with Candidiasis of the nipples. The study was done at two hospitals in Australia; and, involved 360 women who were pregnant for the very first time. Researchers followed up on the women at six different times: in the hospital, weekly at home visits until 4 weeks postpartum, and via telephone at 8 weeks after childbirth. The study found, that Candida infection of the nipple, is associated with burning nipple pain and breast pain. Yet, the study also cautions not to jump to conclusions when you have pain in the breast or nipple. The researchers state that women with nipple damage or vasospasm (sudden constriction of a blood vessel, reducing its diameter and flow rate) can experience burning pains; and, has sometimes led to a misdiagnosis of Candida infection. The study explains, that the pain associated with Candida infection, is persistent, ranges from mild to severe, and does not go away by using nipple shields, switching to breast pumping, or through the application of heat. And, pain can be related to a baby’s feeding—the cause being mechanical in nature. If your nipple and breast pain goes away when you apply heat to the area, vasospasm is the probable cause of the pain. The researchers also found that nipple damage could be accompanied by burning nipple pain and radiating breast pain. Therefore, one should be cautious about assuming Candida as the cause, when such damage is present.
A study, published in the Canadian Family Physician [40 (1994): 1407], describes in detail the process they used to diagnose women with a nipple yeast infection. The following three criteria were used to diagnose nipple Candidiasis:
- Intense, burning pain in the nipple or areola that increases in severity after feedings; and, continues for a minimum of 15 minutes after feeding. The start of this pain must be after the first postpartum week. Pain from Candida, unlike pain from nursing trauma, will not improve with better feeding practices.
- Deep, shooting pains that radiate through the breast. These pains can happen while feeding and between feedings.
- Purple, or red, discoloration of the areola or nipple.
If you find yourself with breasts that exhibit some, or all, of the symptoms mentioned by these studies to indicate nipple thrush, you may also want to consider predisposing factors of this condition. If you happen to have some, or all, of the predisposing factors of this nipple infection, and you have the symptoms that accompany it; a diagnosis of Candidiasis of the nipple is all the more likely.
Eliminate Bacterial Vaginosis & Vaginal Odor
Jennifer O’Brien is one prominent expert on BV that knows how to get rid of vaginal odor. BV is a common infection that you don’t have to put up with.
Jennifer will show you how to naturally eliminate vaginal odor in just 3 days.
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Predisposing Factors

A very comprehensive analyses, of what actually can cause a nipple yeast infection, was given by a study published in the Journal of Human Lactation [7.4 (1991): 177-181]. The study employed a survey to determine possible causative factors of thrush on the nipples. The survey was given to 51 women who had thrush on their nipples, 18 women experiencing other problems during their breastfeeding, and 29 women who were not having any problems with breastfeeding. The study determined, that the primary correlations with nipple Candidiasis, included: antibiotic therapy after birth, previous history of long-term antibiotic therapy, damage of the nipples in early lactation, and a history of vaginal yeast infections. The study also found, not surprisingly, that oral thrush was more prominent in babies whose mothers had nipple thrush.
Concerning the aforementioned Canadian Family Physician [40 (1994): 1407] study; this research also tried to address the issues behind women getting nipple yeast infections. This research involved 105 different women; 27 who were positive for nipple Candidiasis, and 78 who did not have any nipple Candidiasis. The study found there was a correlation between nipple thrush and three factors: vaginal yeast infections, nipple trauma, and previous antibiotic drug therapy. Therefore, this study also agrees with the Journal of Human Lactation [7.4 (1991): 177-181] study; in that, these same three factors, seem to elevate risk for nipple thrush.
The following chart, was taken from the Canadian Family Physician [40 (1994): 1407] study, and shows the number of women who reported having certain factors that would predispose them to nipple thrush. The case group in the chart are those women who met diagnostic criteria for nipple thrush; and, the control group women did not have nipple thrush. The letter ‘N’ signifies the number of women.
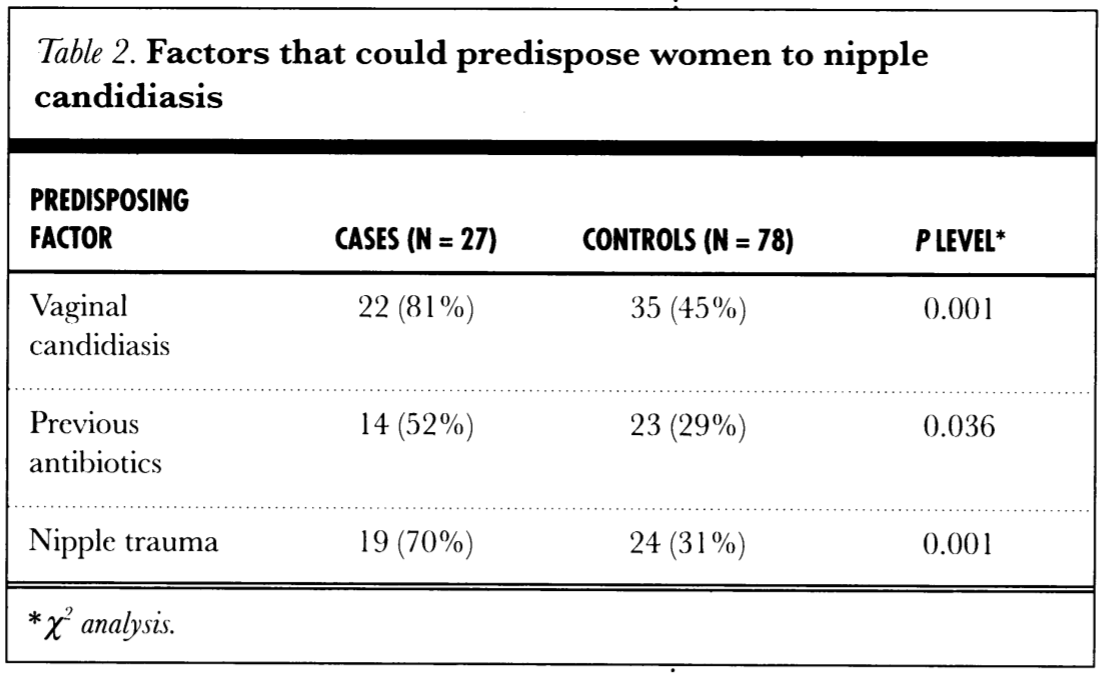
In this study, all of the babies of the 78 women in the control group (who did not have nipple yeast infections) also did not have any diaper rash or oral thrush. Yet, 48% of the babies of the women with nipple Candidiasis, were diagnosed with diaper rash; and, 38% of these babies had visible oral thrush. Thus, it is important to treat your baby for Candidiasis—if you have a nipple yeast infection. Also, properly cleaning the nipples, pacifiers, and anything else routinely in the baby’s mouth is important to limit the spread of Candida. By prohibiting yeast from colonizing the baby's mouth, or the mother’s nipples, incidence of infections in these areas, can be decreased.
Clair Goodall: Author & Nature Lover
Clair Goodall is a bee-obsessed natural medicine convert from Minnesota. She is one expert you might want to know more about!
Clair will help you protect you and your family from toxic products and chemicals and help you discover solutions from nature.
Also, Clair’s book is backed by a 60-day, 100% money back guarantee
Visit Official Site!Natural Nipple Yeast Infection Remedies
Treating an outbreak of Candida on the nipple, is just like treating a yeast infection of the skin. What you will want to do, is to get some coconut oil and mix in some essential cinnamon oil, essential oregano oil, and essential lemongrass oil. Mix the oils together; and, you will then need to apply it to the nipple and area of the breast that Candida is currently attacking. You may want to get some absorbent material and soak the oil mixture in it; and, then use some tape to keep it in contact with your nipple. Change the soaked pad about 2 times a day to keep up the attack on Candida. If you feel discomfort while performing this procedure, discontinue and wash the oils off. You can try a weaker concentration of essential oils at a later time.
Coconut oil, and these three essential oils, all are antifungal; and, will start killing the yeast attacking your nipple. Mixing up three different essential oil is likely going to be more powerful than using just one essential oil; as there can be a healing synergy created when multiple phytochemicals attack a pathogen.
You should make sure to thoroughly clean off your nipple and breast before you feed your baby. Coconut oil, by itself, shouldn’t cause any problems; yet, essential oils are not safe to give to a baby. So, clean off your nipples with soap and water to remove any traces of essential oils before you feed your child. Also, try and avoid using tea tree oil to treat a nipple yeast infection, if you are breastfeeding. Small amounts of tea tree oil can be lethal to adults when ingested.
Get Kate Hale’s Support
Recommended by Dr. Anne MacGibbon, Obstetrician and mother of three, Kate Hale delivers valuable nuggets of wisdom on breastfeeding essentials.
Kate shows you a complete and effective technique that will teach you to deeply latch your baby and breastfeed without pain within minutes for a contented baby and an end to sore nipples.
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Other Remedies for Nipple Pain
One fairly comprehensive examination of treating nipple pain, in mothers who were breastfeeding, was published in the International Journal of Environmental Research and Public Health [12.10 (2015): 12247-12263]. The study looked at 264 breastfeeding mothers who were experiencing nipple pain. The study found that the instigation of nipple pain was due to multiple factors in 89% of these cases. The three most frequent factors causing nipple pain were incorrect positioning (238 women), ankyloglossia (baby being tongue tied—177 women), and the baby having an unusual palat (117 women). Candida infection was suspected in just 7 women; and, only 6 women used an antifungal. Of the women who took an antifungal, only half were healed or had improved.
The study reported, that incorrect positioning of the child during breastfeeding, is the primary cause of nipple pain. If you are unsure you are breastfeeding correctly, and you are having nipple pain, you may want to get some instruction. If your baby has a high arched or bubble palate (palatal anomaly), or is somewhat tongue tied, using a breast pump and bottle, instead of direct suckling, could resolve your nipple pain.
Professional Guidance & Help with Breastfeeding

If you have been having some difficulties with breastfeeding, and this is leading to pain or skin agitation, you may want to get some expert advice on how to do this. Unfortunately, many first time moms can struggle with this important, bonding experience. Fortunately, there are women like Kate Hale who can give a lot of help, and support, to moms desiring to improve their breastfeeding. Kate Hale is a registered nurse, registered midwife, and International Board Certified Lactation Consultant. She has spent over 25 years in postnatal care in her private practice and in maternity hospitals throughout Australia. Kate can guide you in helping your baby latch and feed; so you can reduce the amount of mechanical stress exerted on your nipples. Kate offers a series of informative videos that guide moms in breastfeeding and several other topics—such as avoiding mastitis. You will be able to steer clear of breast thrush more easily using proper nursing techniques. If you’d like to learn a bit more about Kate and her program, you can find out more at Kate Hale’s website.
A Natural, 12 Hour Yeast Infection Cure

According to a research paper published in Clinical Microbiology Reviews [12.1 (1999): 80-96], Candida species are quite ubiquitous organisms. Candida are most frequently present in the mouth; and, live in 31% to 55% of healthy people. The species that causes approximately 70% to 80% of all Candida infections is C. albicans.
The Chinese Journal of Obstetrics and Gynecology [2011 Jul;46(7):496] reports there appears to be a correlation between intestinal Candida infections and vaginal yeast infections. And, this provides a clue, as to why yeast infections in general, can reoccur.
This study states, in 148 cases of vaginal candida infections, 33.1% of the women were infected in both the intestines and vaginal area. The recurrence rate of yeast infections, in women with simultaneous intestinal infection, was significantly higher than for women who did not have an intestinal infection. This study concluded that vaginal yeast infections are highly associated with simultaneous intestinal Candida infection.
As research appears to indicate, systemic Candida infections can and do happen. A more systemic Candida infection may primarily get a foothold in the intestines; and cause a wide array of problems. If your yeast infections keep happening, a systemic Candida problem may be why.
One woman who suffered from a systemic Candida infection, for about 12 years, was Linda Allen. The systemic Candida infection that attacked Linda caused a wide range of health problems in addition to yeast infections. Some of these problems, Linda describes in her own words in the following quote:
To be honest, it was hard to pinpoint exactly what was wrong: I wasn’t really sick, but I wasn’t really well either. I had listlessness, fatigue, brain fog, stomach ailments, unexplained rashes, skin infections, and so on. It seemed like every day brought a new challenge.
My energy was sapped and I felt exhausted, which affected my grades and put a big dent in my social life.
Linda Allen’s symptoms included an embarrassing vaginal discharge, severe itching, and burning sensations. Her infections were difficult to deal with, and Linda’s health problems cost her financially as well. Linda states these infections of Candida can become excruciating when they happen as frequently as a menstrual period.
Yet, Linda spent a great deal of time in research; and even questioned health professionals who were kind enough to share some time with her. Linda even tried an array of purported "cures." Although it took a while, eventually, Linda put together a natural treatment plan she hoped would solve her Candida situation.
After spending about a year refining her new approach, Linda tried her system on herself. It worked amazingly well. Linda even returned to a few medical doctors to get tested for the presence of infections. These tests revealed all indicators of infection had vanished! Linda was indeed well again, after such a long, difficult journey.
Linda has since published a book detailing how to copy her success. She also includes a 12 hour yeast infection cure that can get rid of a superficial (such as a genital yeast infection or oral thrush) yeast infection in about 12 hours.
Linda’s publisher protects those who get her book with a 60 day, 100% money back guarantee. Linda’s publisher, a subsidiary of the United States based firm Keynetics Incorporated, is a reputable digital retailer that has been around for a long time. They have great customer service, and make getting a full refund on Linda’s book quick and easy. If you’re not satisfied, you can quickly get all your money back.
If you would like to learn more about Linda’s journey to freedom from Candida, see reviews of others who tried her natural system, or find out more about her efficacious book; you can find more information at Linda Allen’s website.
Author: Mr. Nicholas Gross

Nick Gross is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Nick is primarily a web developer but also researches and authors written and video content about natural health. Nick has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Affiliate Disclosure
Some of the links provided on this website are affiliate links. When a purchase is made through these links, Candida Hub earns money from commission. This helps to keep the website up and helpful to people for free. Thank you for any support!
Stay Up to Date
If you enjoyed this article, consider following / liking our Facebook page. This page is primarily utilized to alert followers of new articles that are put on Candida Hub. Candida related news is also discussed. While you are there, you can see what has been more recently added to Candida Hub.
SOURCES:
- http://dx.doi.org/10.1136/bmjopen-2012-002351 — Amir, Lisa H., et al. "Does Candida and/or Staphylococcus play a role in nipple and breast pain in lactation? A cohort study in Melbourne, Australia." BMJ open 3.3 (2013): e002351. Full Text Available Here
- http://dx.doi.org/10.1177/089033449100700414 — Amir, Lisa Helen. "Candida and the lactating breast: predisposing factors." Journal of Human Lactation 7.4 (1991): 177-181. PubMed
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2380126/ — Tanguay, Karen E., Mary R. McBean, and Evelyn Jain. "Nipple candidiasis among breastfeeding mothers. Case-control study of predisposing factors." Canadian family physician 40 (1994): 1407. PubMed PDF
- http://dx.doi.org/10.3390/ijerph121012247 — Kent, Jacqueline C., et al. "Nipple Pain in Breastfeeding Mothers: Incidence, Causes and Treatments." International journal of environmental research and public health 12.10 (2015): 12247-12263. Full Text Available Here, PubMed Full Text
- https://doi.org/10.1128/CMR.12.1.80 -- Fidel, Paul L., Jose A. Vazquez, and Jack D. Sobel. "Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans." Clinical Microbiology Reviews [12.1 (1999): 80-96].
- https://pubmed.ncbi.nlm.nih.gov/22041440/ -- Lin XL, Li Z, Zuo XL. "Study on the relationship between vaginal and intestinal candida in patients with vulvovaginal candidiasis." Chinese Journal of Obstetrics and Gynecology (Zhonghua fu chan ke za zhi). [2011 Jul;46(7):496].