See all "Birth Control" Section Topics

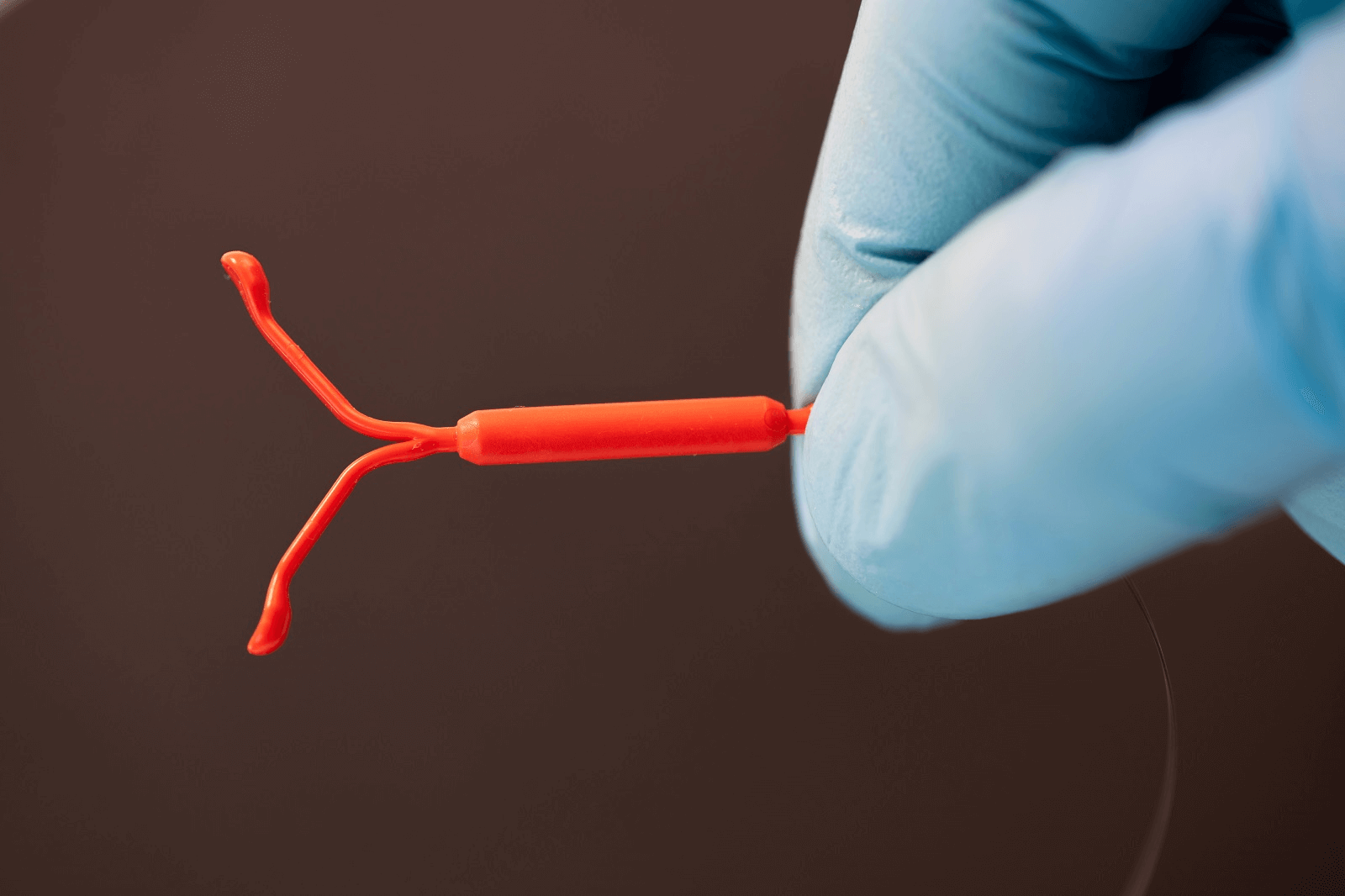
As research appears to indicate, there is likely not a direct correlation between vaginal yeast infections and using an intrauterine device (IUD). As will be discussed, one study, encompassing 600 women participants, found that using IUDs does not present a statistically significant increase in the risk for having a yeast infection.
Yet, this same study stated that Candida (Candida is the genus of yeast that causes all yeast infections) is an opportunistic pathogen (it causes an infection when it is presented with an opportunity to overgrow and do so), and long term usage of an IUD can cause conditions in the vagina to become favorable to Candida overgrowth.
Concerning just the presence of Candida in the vagina, even if it might not be causing a noticeable infection, IUD use can influence this. Research suggests that IUD use is a strong predisposing factor to having Candida in the vagina. Yet, Candida is commonly found in humans and often does not cause an infection.
Candida is a commensal organism most of the time; i.e., it gains a benefit from a host while not benefiting that host or causing it harm (Sanna E. and Kumamoto; 2014). Therefore, just because you have Candida in your vagina, you are not guaranteed to have an infection. Candida can live in the vagina without causing an infection; but, because it is an opportunistic pathogen, it can overgrow and cause a problem when conditions for this are right.
Candida can adhere to IUDs and form a biofilm on these devices. One study’s findings tend to favor the assumption that the tail of an IUD can act as a reservoir and prevents the mucus membranes (the membranes lining the interior of the vagina) from clearing away yeast cells. Thus, given that Candida can effectively attach to IUDs, these devices may be able to instigate yeast infections; or play a role in recurrent yeast infections.
Of course, there does not seem to be much, if any, research that found a direct correlation between IUD use and yeast infections.
On an individual basis, a woman might actually get yeast infections from an IUD that is inhabited by Candida. This is certainly within the realm of possibility. Although this does not appear to be common enough to yield a statistically significant correlation in studies; this is not a guarantee that IUDs never cause yeast infections.
One study even suggested their research indicated that the presence of Candida biofilm on an IUD was an important risk factor for recurrent vaginal yeast infections.
It may be that if you have some condition or situation that predisposes you to vaginal Candida overgrowth, having an IUD may increase your odds for developing a yeast infection. As research will indicate, IUDs may impart 4.25 times the risk for having Candida in the vagina. And, when Candida is in the vagina, it only takes the right situation to occur and then you will end up getting a yeast infection.
Possibly a key thing to consider is the timing of your yeast infections. If you seem to get yeast infections after the insertion of an IUD—and not before—it may be that the IUD is harboring Candida; and, conditions in your vagina are favorable to Candida overgrowth.
If you cannot address the issues that may be predisposing you to infection (such as a lack of good probiotic Lactobacilli in the vagina, ceasing to take estrogen hormone based drugs, or stopping the use of strong antibiotics), removing the device may actually stop the yeast infections.
Again, there is no clear statistical correlation between IUD use and yeast infections; yet, individual situations may not always concur with statistical models. Consequently, it is hard to tell if removing an IUD will help; but it is a good guess that in special situations device removal certainly could.
A 1/2 Day & Yeast is Gone!
Linda Allen suffered from yeast infections for years. Through researching natural medicine & Candida, she found an efficacious solution!
Linda is one expert you want on your side! Let her show you how to get rid of a superficial yeast infection in just 12 hours; AND, keep it gone!
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Research Related to IUDs & Yeast Infections

The first study we will examine, was published in the Central European Journal of Public Health [13.1 (2005): 32]. According to the study, it is well understood that the presence of a foreign body, such as an IUD, alters the vaginal microbiome to favor anaerobes, can disturb the microbiological life in the vagina, reduces Lactobacilli population, and can prepare the environment for Candida overgrowth.
One reason this study was done, was to better understand the possible interaction between IUD usage and Candidiasis.
The study utilized 600 women; among them were 56 IUD users and 544 non-users. Among the 56 IUD users, 8 women (14%) had a yeast infection. Among the 544 non-users, 44 women (8%) had a yeast infection. The research indicated that there was not a statistically significant correlation between IUD usage and yeast infections.
Thus, the study indicated that IUD’s do not cause yeast infections. However, this study also reported that there was a correlation between longer IUD usage and the presence of more hyphal form Candida cells.
Hyphal cells are long germ tubes that the round Candida cells (blastoconidia) transform into. Hyphal germ tubes allow Candida to burrow into tissue and attach to that tissue to a greater degree. Hyphal form Candida growth indicates that the yeast is in a more pathogenic mode of growing. The authors of the study stated (note: IUD is abbreviated IUCD):
In conclusion we observed that Candida infection is a frequent problem of women and also its prevelance is relatively high in IUCD users although the correlation between Candida and IUCD is not significant according to the 𝛘2 test. Since this fungus is an opportunistic normal cervico-vaginal flora microorganism, it will overgrow and begin filamentation as soon as the conditions are favorable for Candida. According to our data these conditions are obtained by the long-term usage of IUCD which supported the expansion of more pathogenic "hyphael" form.
Central European Journal of Public Health [13.1 (2005): 32]
The next study we will investigate was published in BJOG: An International Journal of Obstetrics & Gynaecology [95.4 (1988): 408-410]. Two primary questions this research sought to answer were: does an IUD predispose a woman to get yeast infections; and, does an IUD increase the prevalence of Candida in women who use an IUD?
To arrive at answers, the research analyzed 117 women who used an IUD and 100 women who did not use an IUD (serving as a control group). These female participants were those who went to a gynaecologist for the sole purpose of having a routine check-up. None of the women who were tested in the study had factors at the time assumed to predispose them to yeast infections; i.e., none of them had taken antibiotics or corticosteroids in the previous two months, no steroid contraception was used, none were pregnant, and none had diabetes.
The study also examined the women for the presence of signs or symptoms associated with vaginal Candidiasis; i.e., inflammation, vulvar itching, cottage cheese like vaginal discharge, or discharge that was heavier than normal.
The study found that 23 IUD users had yeast cells in their vagina. Concerning women that did not use IUDs, only 6 women had yeast isolated from their vaginas. This difference in the presence of yeast was statistically significant. Concerning the presence of signs and symptoms suggestive of vaginal Candidiasis, 14 IUD users had them; and, 3 non-IUD users had them. This difference was also statistically significant.
The study also found that about 50% of IUD users and 66% of non-IUD users that had yeast in their vaginas were without symptoms.
The study concluded by stating their findings strongly suggest IUD use is a predisposing factor to the presence of Candida in the vagina. And, in half the women the presence of yeast in the vagina was not associated with signs and symptoms of infection. The study also said their findings tend to favor the assumption the tail of an IUD acts as a reservoir and prevents the mucus membranes from clearing away yeast cells.
The next study we will investigate was published in the Journal of Obstetrics and Gynaecology Research [45.2 (2019): 438-442]. The study sought to see the prevalence of Candida in the vagina before and 3 months after the insertion of a copper IUD. The study had 122 women participate in the research; yet, overall only 95 women finished the study.
The participants were healthy, aged 16 to 50 years, and chose to have an IUD for contraception. The participants also had no history of systemic or local use of antibiotics or antifungals in the previous two weeks.
The study found that only before insertion of the IUD, 4 women had positive laboratory cultures for Candida; yet, they did not appear to have any vaginal infection. Seven women had positive Candida cultures both before and after insertion of the IUD. After insertion of an IUD, 17 vaginal cultures were positive for Candida. The research reports that Candida positive test results were significantly increased 3 months after IUD insertion.
Concerning the species of Candida that caused the infections in both tests (before and after IUD insertion), 51.4% of these cultures were Candida albicans (C. albicans); 31.4% were C. glabrata; and, 17.1% were concomitant infections of C. albicans and C. glabrata.
Concerning the risk using an IUD imparted for a positive laboratory culture of Candida, it was quite high. The study found an odds ratio (OR) for having a positive laboratory culture after IUD insertion of 4.25. This means that an IUD made the women in the study 4.25 times as likely to have a positive laboratory culture for Candida.
An odds ratio shows how likely an event is given a particular variable. In this case the event is a positive Candida culture; and, the variable in question is if a woman is using an IUD.
Before any of the women had an IUD inserted, none of them had any clinically observable vaginal yeast infections. And, having a vaginal infection is one reason not to have an IUD inserted while the infection is there. Yet, three months after the women had IUDs inserted, of the 24 women with a positive Candida culture, only 14 women had signs of an infection (such as inflammation of the vulva, vaginal discharge, and itching).
Eliminate Bacterial Vaginosis & Vaginal Odor
Jennifer O’Brien is one prominent expert on BV that knows how to get rid of vaginal odor. BV is a common infection that you don’t have to put up with.
Jennifer will show you how to naturally eliminate vaginal odor in just 3 days.
A 60-day, 100% money back guarantee is provided.
Visit Official Site!IUDs & Candida Biofilm
A study, published in the Journal of Antimicrobial Chemotherapy [67.3 (2012): 618-621], describes the importance of understanding Candida biofilm quite well. According to this study, Candida cells protected by a biofilm (known as sessile cells) are 1024 times or more resistant to antifungal drugs—compared to cells not protected by biofilm.
The study also relates that the majority of yeast infections are associated in some way with Candida biofilms forming on a biological or inert (e.g., a medical device) surface. The following quotation was taken from the study and illustrates, in the author’s own words, the critical nature of Candida biofilm:
The majority of manifestations of candidiasis are associated in one way or another with the formation of Candida biofilms on the surfaces of inert or biological surfaces. Sessile (biofilm) cells display unique phenotypic traits in comparison with planktonic cells. The most notable of these is that sessile cells are notoriously resistant to antimicrobial agents and withstand host immune defences, and this is the main reason why biofilm-associated infections are frequently refractory to conventional antibiotic therapy.
Journal of Antimicrobial Chemotherapy [67.3 (2012): 618-621]
A study, published in Frontiers in Medicine [5 (2018): 28], discusses Candida biofilms. The research states that a biofilm is comprised of a community of microorganisms that are irreversibly attached to a surface; this surface can be some material or biological tissue. The biofilm produces extracellular polymers (a secreted, sludge like material) that serve a structural purpose.
The microorganisms in a biofilm have a lower growth rate and much higher resistance to artificial drugs. The capability of a microorganism to adhere to different kinds of surfaces allows them to form a biofilm on medical devices (such as an IUD or catheter). The study states that 80% of microorganisms live in biofilm.
So, understanding the importance of Candida biofilm, let’s examine some of the studies relating to this biofilm formation on IUDs.
Candida Biofilms Develop on IUDs
A study, published in Medical Mycology [48.1 (2010): 211-216], sought to investigate the presence of biofilm on the surface of IUDs in women with recurrent yeast infections. The research also tried to determine the susceptibility of yeasts they isolated to amphotericin B and fluconazole (both are synthetic antifungal drugs—amphotericin B brand names include Abelcet and Ambisome; and, fluconazole has the brand name of Diflucan).
The study utilized two patients with symptoms of recurrent vaginal yeast infections—defined as at least 4 episodes in a year’s time. The first case was a 29 year old woman, who was married, and had two children. This woman was examined and found to not have HIV or diabetes. This woman had used an IUD for 3 years and 1 month as a contraceptive method. The woman said her symptoms started shortly after the insertion of the IUD.
The second case was a 38 year old woman, who was married. The woman had symptoms of a yeast infection; such as cottage cheese like vaginal discharge and itching. This woman was also examined and found to not have HIV or diabetes. The woman had used an IUD for about 5 years as a contraceptive measure. The woman stated her vaginal discharge and itching had become worse over the previous two years.
With the use of a scanning electron microscope, it was determined biofilm was present, with a dense multi-layered network of cells of different microorganisms, on both women’s IUDs. The study also cites other research on IUDs that found biofilm with a mixture of microbes on IUDs.
The study stated that if microbial biofilms form on the surface of IUDs, this may predispose a woman to infection. In the study’s abstract, the authors state their findings indicated that the presence of biofilm on the surface of IUDs is an important risk factor for recurrent vaginal yeast infections.
Another study examined biofilm formation on IUDs. The research was published in the Indian Journal of Microbiology [48.4 (2008): 438]. The authors of this research said one of their goals was to explore the nature of biofilm formed during C. albicans infection in gynecologic infections of women who used IUDs.
According to the study, the effectiveness, safety, and acceptability of IUDs (at the time of this study) made IUDs the most popular reversible contraceptive method; and, IUDs are used by millions of women in the world. Despite being a cost effective contraception solution, the study states research has shown IUD use can lead to heavier periods, menstrual cramps, an increase in the risk of pelvic inflammatory disease, and can cause problems related to the colonization of microbes on these devices.
Additionally, an increase of Candida infections, in the decade prior to this research, had almost paralleled the increase and ubiquitous use of implanted medical devices—mainly in people with impaired defenses.
In this study, the researchers collected infected IUDs from a hospital and local nursing homes. These IUDs came from women suffering from reproductive tract infections. The investigation revealed that infected IUDs from patients with reproductive tract infections had Candida biofilm on them; which was comprised of a single or multiple species.
The C. albicans isolates that were obtained from the IUDs were tested for their ability to form biofilm at different time intervals. These time intervals ranged from 8 to 72 hours. The in-vitro activity of of the antifungal drugs chlorhexidine, fluconazole, amphotericin B, and nystatin against pre-formed Candida biofilm demonstrated an increased resistance to these drugs compared to Candida cells without biofilm.
The authors of this study stated their findings strongly support the argument that patients with reproductive tract infections are more likely to acquire a C. albicans biofilm related infection due to a higher resistance to antifungal drugs.
This research stated that uterine secretions, in normal conditions, actively handle microbes in the vagina and surrounding areas of the female reproductive tract. Yet, an IUD can provide an ideal way for microbes to develop and overgrow as biofilms on these devices. Thus, this research shows IUDs can provide a mechanism for Candida to colonize the vagina.
Clair Goodall: Author & Nature Lover
Clair Goodall is a bee-obsessed natural medicine convert from Minnesota. She is one expert you might want to know more about!
Clair will help you protect you and your family from toxic products and chemicals and help you discover solutions from nature.
Also, Clair’s book is backed by a 60-day, 100% money back guarantee
Visit Official Site!A Natural, 12 Hour Remedy for Yeast Infections

Yeast infections, as much research shows, affect nearly 75% of all women during the course of their lives. And, a small number of these women will develop recurrent yeast infections; typically defined as 4 or more episodes in a year’s time. Recurrent yeast infections can be very disruptive to a person’s quality of life; and, can bring about a lot of financial expenses. Also, when enough yeast is present within the body, it can lead to a wide array of detrimental health issues.
It may be difficult to understand what exactly is happening to your health, if Candida is causing such health problems and you do not know that it is.
One woman who suffered from recurrent yeast infections, and the terrible health consequences of a systemic yeast infection, was Linda Allen. Linda spent about 12 years of her life suffering with Candida related health problems. Linda’s health was affected by Candida; and, she simply did not know what was causing her health issues.
Linda’s ill health would end up costing her a small fortune in medical bills; yet, the doctors did not know how to solve her ailments. This was likely a very frustrating time in Linda’s life.
Linda’s situation did eventually change for the better when she visited a naturopath. Unlike Linda’s doctor, the natural path was able to correctly diagnose Linda’s disease. The naturopath informed Linda that she had Candida overgrowing in her body, and this was the cause of her terrible health.
Once Linda understood her opponent, Candida, she began to invest a great amount of time in researching this condition. Linda read many books and even tried many purported treatments for Candida. She would ask medical professionals for advice, when they were able to afford her some of their time.
Eventually, Linda developed a system based on natural medicine that she hoped would eliminate the Candida in her body. Linda would spend about a year refining her new system before she tried it.
When Linda started her new, natural system; she found that her recurrent yeast infections stopped. In time, Linda’s natural approach would also eliminate the Candida from her body—giving her back her good health. It took a lot of work, but Linda was able to develop—through her knowledge of natural medicine—a safe way to naturally eliminate Candida from the body and permanently stop yeast infections.
Linda’s doctor gave her the suggestion to show her work to others, and Linda did just that. It was not long before Linda had seen the same results she experienced evident in others who tried her protocol. Linda had regained her health, and she found others also were arriving at total freedom from Candida; this was the amazing product of all her hard work.
Linda Allen has since written an entire book detailing her natural treatment plan to eliminate Candida. In her book, Linda also includes an efficacious method for getting rid of a yeast infection naturally in 12 hours of time. Through using Linda’s system, you can eliminate a yeast infection in just half a day.
It is likely going to take longer for people to get free of more systemic types of Candidiasis, yet Linda’s program will work; and give those who try it freedom from yeast overgrowth in their bodies.
Linda’s book is published with a large digital retailer; a subsidiary of the United States based company Keynetics Incorporated. Linda’s publisher also provides a 60 day, 100% money back guarantee on her book. Linda’s publisher also makes the purchasing process safe and easy; and the same is true about the refund process.
For those who decide to try Linda Allen’s book, they can be assured that they can quickly get a full refund of their money if they find the book unsatisfactory. Additionally, Linda Allen’s book is made available as a downloadable PDF format; you will be able to read it easily on your computer or mobile device.
To learn more about Linda’s personal story, to see reviews of those who gave her book a try, or to find out more about her book; you can get more information at Linda Allen’s website.
Author: Mr. Nicholas Gross

Nick Gross is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Nick is primarily a web developer but also researches and authors written and video content about natural health. Nick has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Affiliate Disclosure
Some of the links provided on this website are affiliate links. When a purchase is made through these links, Candida Hub earns money from commission. This helps to keep the website up and helpful to people for free. Thank you for any support!
Stay Up to Date
If you enjoyed this article, consider following / liking our Facebook page. This page is primarily utilized to alert followers of new articles that are put on Candida Hub. Candida related news is also discussed. While you are there, you can see what has been more recently added to Candida Hub.
SOURCES:
- https://doi.org/10.1007/s12281-014-0178-x — Herwald, Sanna E., and Carol A. Kumamoto. "Candida albicans niche specialization: features that distinguish biofilm cells from commensal cells." Current Fungal Infection Reports [8.2 (2014): 179-184].
- https://pubmed.ncbi.nlm.nih.gov/15859178/ — Demirezen, S., O. O. Dirlik, and M. S. Beksaç. "The association of Candida infection with intrauterine contraceptive device." Central European Journal of Public Health [13.1 (2005): 32].
- https://doi.org/10.1111/j.1471-0528.1988.tb06615.x — PAREWIJCK, WALTER, et al. "Candidiasis in women fitted with an intrauterine contraceptive device." BJOG: An International Journal of Obstetrics & Gynaecology [95.4 (1988): 408-410].
- https://doi.org/10.1111/jog.13844 — Moradi, Raheleh, Mamak Shariat, and Lida Moghaddam?Banaem. "Effect of intrauterine device insertion on Candida species in cervicovaginal specimen identified by polymerase chain reaction technic: A longitudinal study on Iranian women." Journal of Obstetrics and Gynaecology Research [45.2 (2019): 438-442].
- https://doi.org/10.1093/jac/dkr512 — Khan, Mohd Sajjad Ahmad, and Iqbal Ahmad. "Antibiofilm activity of certain phytocompounds and their synergy with fluconazole against Candida albicans biofilms." Journal of Antimicrobial Chemotherapy [67.3 (2012): 618-621].
- https://doi.org/10.3389/fmed.2018.00028 — Cavalheiro, Mafalda, and Miguel Cacho Teixeira. "Candida biofilms: threats, challenges, and promising strategies." Frontiers in Medicine [5 (2018): 28].
- https://doi.org/10.3109/13693780902856626 — Auler, Marcos E., et al. "Biofilm formation on intrauterine devices in patients with recurrent vulvovaginal candidiasis." Medical Mycology [48.1 (2010): 211-216].
- https://doi.org/10.1007/s12088-008-0054-x — Lal, Priyanka, et al. "Biofilm formation by Candida albicans isolated from intrauterine devices." Indian Journal of Microbiology [48.4 (2008): 438].