See all "Birth Control" Section Topics
If it appears that stopping birth control pills caused a yeast infection, this could in fact be the case. Yet, it is hard to know for sure, as you may have just come down with an infection by chance; and, this chance infection occurred after you stopped birth control pills. Yet, that situation is perhaps rare; and, therefore it can be speculated that the cessation of birth control really did cause your infection.
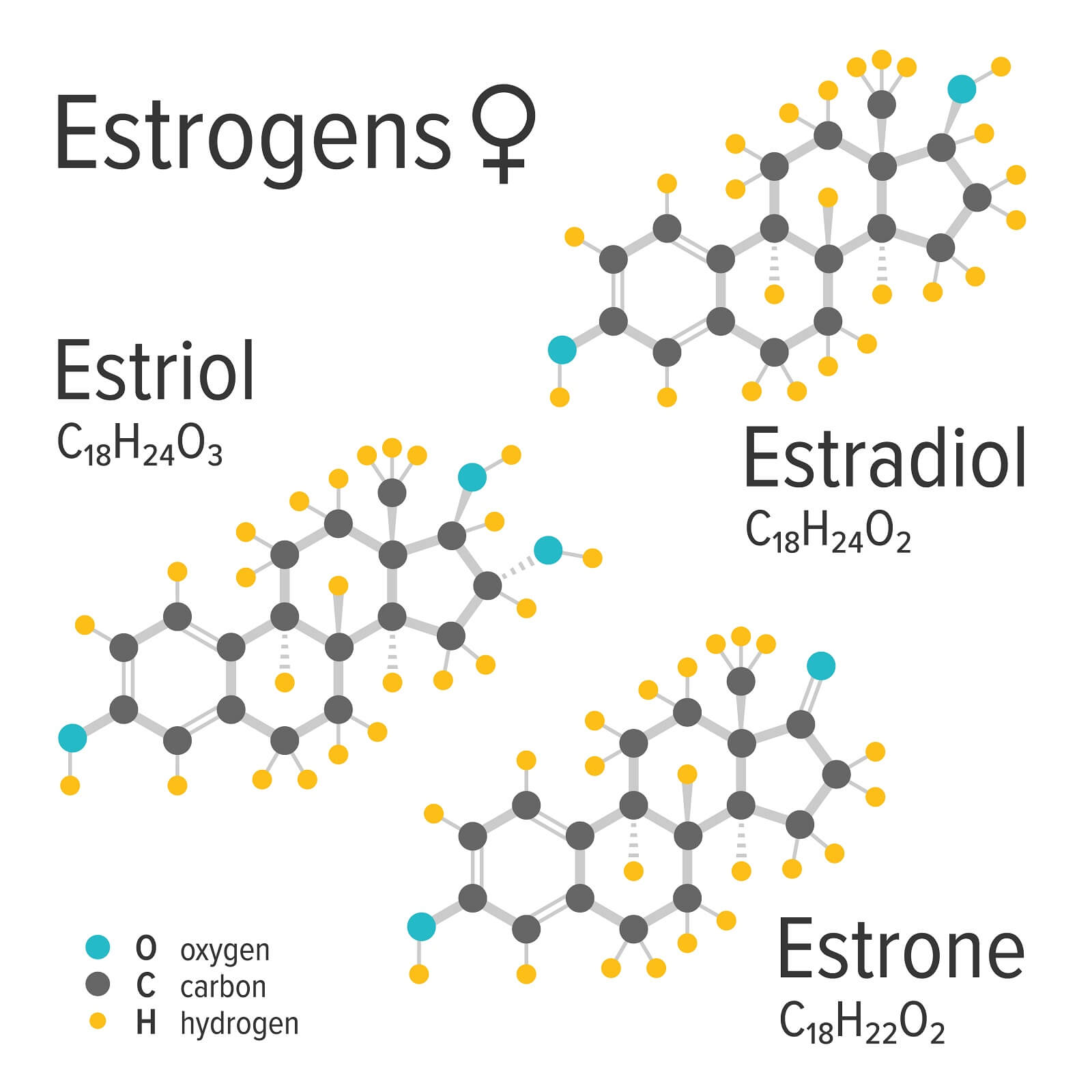
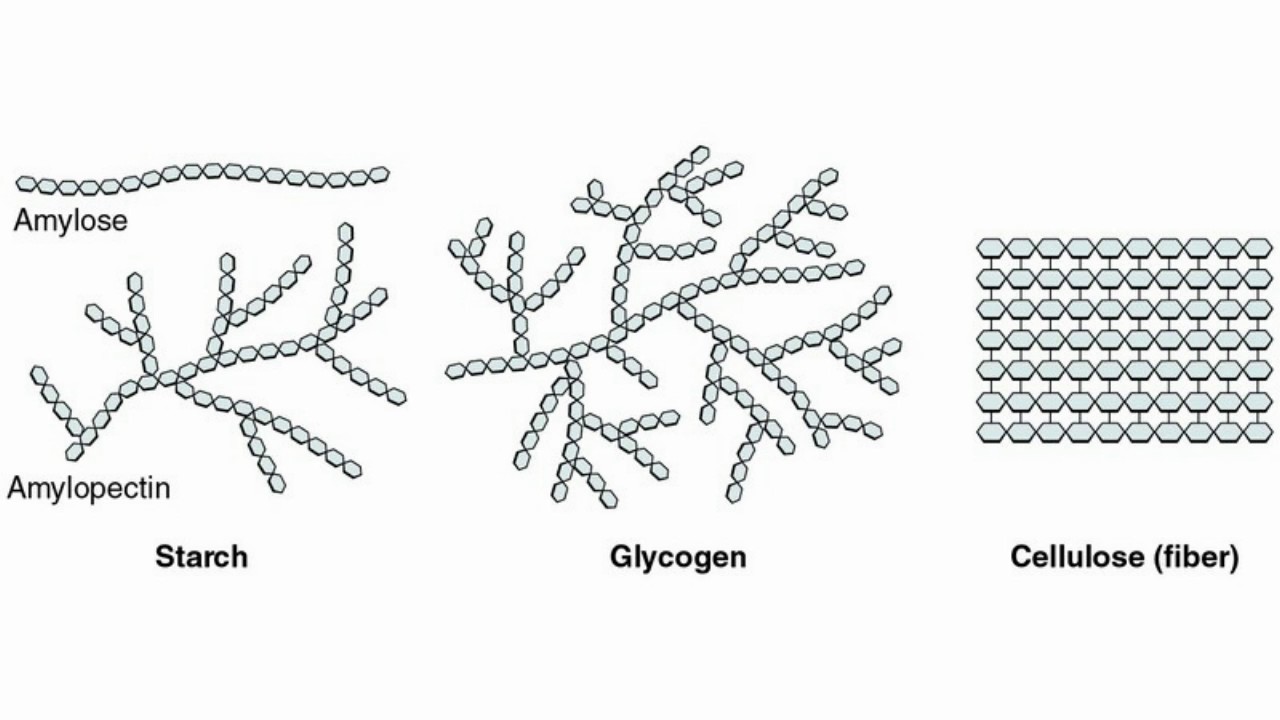
So how would stopping birth control pills cause a yeast infection? Possibly the primary reason this outcome was arrived at, was due to the loss of estrogen. Many birth control pills contain estrogen; when they are taken, this can elevate the levels of this hormone in the body. Estrogen is a critical hormone which causes the vaginal tissue to take on glycogen. Glycogen is a complex carbohydrate that the body uses for energy; it is quite a ubiquitous energy storage molecule. One way the vaginal tissue responds to estrogen is by taking on more glycogen.
So how does the presence of glycogen affect the occurrence of a yeast infection? The answer to this question can be found in the vaginal microbiome (microbiome is a term for the living conditions of microscopic life in a certain area). A healthy woman’s vagina is normally dominated by Lactobacilli bacteria. Species like Lactobacillus crispatus (L. crispatus), L. iners, and L. jensenii normally flourish in a healthy vagina. They work to eat up carbohydrates in the vaginal microbiome, take up “living space,” (sites where microbes can bind and start growing) and secrete lactic acid via their metabolic processes. The lactic acid these probiotic bacteria secrete helps to keep a woman’s vagina in a healthy, acidic state. Lactobacilli prefer an acidic environment to live in; and this acidic environment helps to keep bad bacteria and yeast in check—stopping them from overgrowing and causing an infection.
Therefore, the proliferation of Lactobacilli bacteria is key for stopping yeast infections. Candida is the yeast that causes all yeast infections; and Lactobacilli can be thought of as natural enemies to this pathogenic fungi. When there are not enough Lactobacilli in the vagina, there is going to be more carbohydrates available for Candida and bad bacteria to consume; as well as more available living space. Also, Candida prefers a more alkaline pH to grow in; and, a higher (more alkaline) vaginal pH is a key predisposing factor to yeast infections. A higher vaginal pH can also lead the way to the most common of all vaginal infections: bacterial vaginosis (BV). Bacterial vaginosis is simply an overgrowth of bad bacteria in the vagina; and, its most notable symptom is foul vaginal odor.
It may be that you are a woman with generally lower levels of estrogen. Each woman’s estrogen levels are different. Some women have high estrogen, and other women have low estrogen. Both high and low levels of estrogen may play a role in getting a yeast infection; yet, it is low estrogen levels that we are probably concerned with here.
Low estrogen levels can cause there to be less glycogen in the vaginal tissue. This means less available food for Lactobacilli. When you take estrogen based birth control pills; no doubt you start having more estrogen in your body than prior to taking the oral contraceptive. In this event, the vaginal tissue might start taking on more glycogen. This glycogen, after it is broken down by an enzyme, becomes food for Lactobacilli. The microbiome of your vagina then became dominated by good Lactobacilli bacteria; and, you were without yeast infections.
Once you stopped taking estrogen containing birth control pills, the following scenario could have transpired: The glycogen levels in the vaginal tissue may have fallen due to a loss of estrogen. You may have been a woman with lower than normal natural estrogen levels to begin with. This, in turn, caused a loss of good Lactobacilli. Your vaginal microbiome then became more alkaline, and allowed for Candida to come in and colonize the area. The result was an overgrowth of Candida that quickly dominated your vaginal microbiome; and, you ended up with a yeast infection.
Bad bacteria may have also overgrown and given you a concomitant BV infection along with the Candida problem. In such an event, you might have even noticed that you ended up with a bad vaginal odor (or foul smelling vaginal discharge); this is a classic symptom of BV.
Again, it is hard to know for sure the exact etiology (cause) for a yeast infection. But, because it happened right after you stopped using birth control pills; the aforementioned scenario is a strong contending theory for what actually happened. Later on in this article, we will discuss some natural solutions for this type of Candida problem.
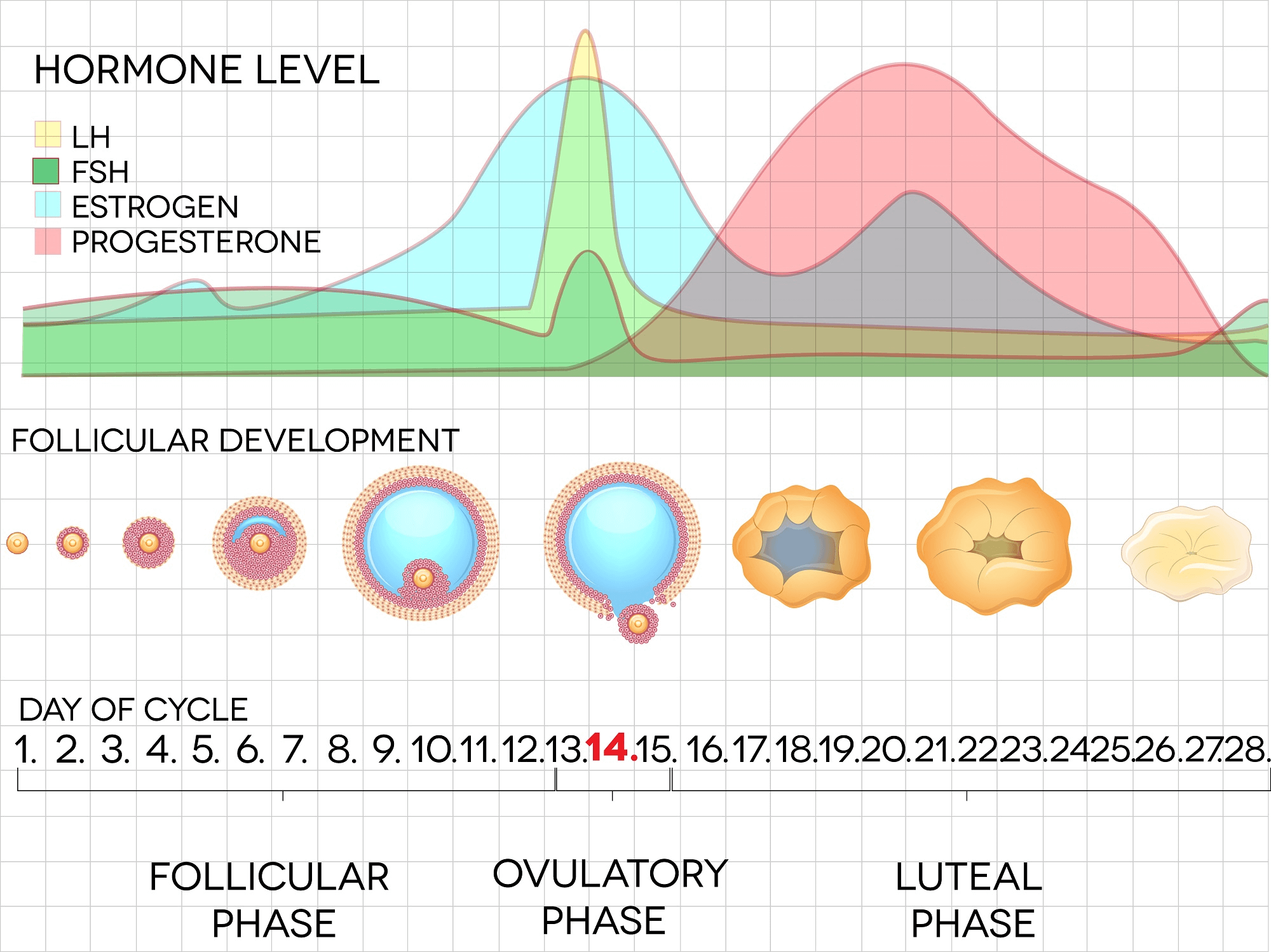
To better illustrate the changes of hormones in the menstrual cycle, the following chart is presented below:
A 1/2 Day & Yeast is Gone!
Linda Allen suffered from yeast infections for years. Through researching natural medicine & Candida, she found an efficacious solution!
Linda is one expert you want on your side! Let her show you how to get rid of a superficial yeast infection in just 12 hours; AND, keep it gone!
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Estrogen, Glycogen, & Lactobacilli Research
The first study we will examine illustrated the point that Lactobacilli rely, to some extent, on glycogen as a food source. The study was published in the Archives of Gynecology and Obstetrics [272.3 (2005): 211-213]. According to the study, the colonization of the vagina by Lactobacilli is facilitated by ovarian hormones in pre-menopausal women. The circulation of estrogen helps to maintain vaginal glycogen levels. When Lactobacilli are present in the vagina, they can produce enough lactic acid from glycogen to maintain the vaginal pH (usually the pH is maintained at 4.0 to 5.0). Menopausal women, due to a reduction in the circulation of estrogen, will see a gradual loss of glycogen and Lactobacilli; this may be accompanied by an increase in vaginal pH (a higher pH is a more alkaline pH).
Another study, published in the Archives of Gynecology and Obstetrics [273.4 (2006): 195-202], discusses the relationship between estrogen and vaginal glycogen content. The study states that changes in the vagina and vulva, during a woman’s reproductive years, are associated with the menstrual cycle and pregnancy. According to the study, the vaginal mucosa (the mucous membranes that line the vaginal vault) responds to changes in ovarian hormone levels. Estrogen stimulation causes the vaginal epithelium (the tissue lining the vaginal vault) to become thicker, and to increase in glycogen content. The glycogen content of the vaginal epithelium is at its maximum at approximately the middle of the menstrual cycle.
An additional study, discusses the relationship between estrogen, glycogen, and Lactobacilli; the study was published in Frontiers in Medicine [5 (2018): 181]. According to the study, the vagina has a plethora of microorganisms in it; these microorganisms exist in a mutualistic relationship (where both species benefit) with the host. Lactobacilli help to augment the defense against colonization of opportunistic pathogens (Candida is an opportunistic pathogen). The composition of the vaginal microbiome is dynamic and goes through changes that correspond to hormonal fluctuations that occur during a woman’s reproductive years.
The study states that a number of protective Lactobacilli species dominate a healthy vaginal microbiome. These include L. jensenii, L. iners, L. gasseri, and L. crispatus. Some anaerobes, that can cause infections such as bacterial vaginosis (BV), are kept in check via the protective action of Lactobacilli.
The study states that rising levels of estrogen promote the accumulation of glycogen in the vaginal epithelial cells. Glycogen is broken down by an enzyme in the body; the carbohydrate components glycogen is broken down into are then utilized by Lactobacilli in metabolism; and, lactic acid is produced. This process creates an acidic vaginal microbiome; with a pH of about 3.5 to 4.5. This acidic pH is prefered by Lactobacilli and helps them maintain dominance in this environment. Yet, Lactobacilli dominance decreases as estrogen levels decline following menopause, and increases with vaginal estrogen replacement therapy. The study states: "In essence, the normal acidic vaginal pH in reproductive-age women is driven by estrogen, glycogen, and Lactobacilli."
Eliminate Bacterial Vaginosis & Vaginal Odor
Jennifer O’Brien is one prominent expert on BV that knows how to get rid of vaginal odor. BV is a common infection that you don’t have to put up with.
Jennifer will show you how to naturally eliminate vaginal odor in just 3 days.
A 60-day, 100% money back guarantee is provided.
Visit Official Site!More Information about Estrogen
One study, published in Endocrinology [76.1 (1965): 63-69], looked at estrogen and how it would influence glycogen synthesis in rats. The research involved the administration of extra estrogen and monitoring the changes in glycogen synthesis in rat uteruses. After the administration of estrogen, the research found:
- Initially, after giving the estrogen, there was a lag phase of less than 2 hours.
- From 2 to 4 hours, glycogen concentrations in the rat uteruses increased at a constant rate.
- At 10 to 24 hours, there was an equilibrium period.
- At about 24 hours after estrogen administration, a decline in glycogen concentration was seen.
The research also stated that the glycogen synthesis, induced by the administration of 1 µg of estrogen (which was 3 to 4 times the levels of estrogen, at 10 to 12 hours, in rats that did not receive extra estrogen), appeared to be the most glycogen the extra estrogen could cause the uteruses to produce. Higher doses of 10 µg of estrogen, or repeated injections of estrogen, did not cause the uteruses to produce more glycogen than the 1 µg dose did. This finding suggested that the maximum stimulation of the glycogenic systems had probably been reached.
Although human women were not tested in this study, it may shed some light onto the fact that female mammals may all respond to some degree to estrogen by the production of glycogen. And, it can be speculated that extra estrogen from birth control pills might further stimulate the glycogen synthesis process in human women.
A study that looked at free glycogen levels; i.e., glycogen that exists outside of cells; and its relationship to vaginal pH and Lactobacilli presence, was published in Menopause [22.7 (2015): 702]. The study collected 82 vaginal fluid samples from 23 women. The amount of free glycogen in in the fluid samples showed a wide distribution; ranging from 0 µg / µL (micrograms / microliter) to 0.487 µg / µL. The samples taken from post-menopausal women had significantly lower amounts of free glycogen than those from pre-menopausal women. Post-menopausal women had an average of 0.002 µg / µL compared to 0.065 µg / µL for pre-menopausal women. The study also found, at the individual level, the amount of free glycogen varied considerably for some women.
The study also examined Lactobacilli in the lower genital tract; and it was theorized that they utilize glycogen as an energy source. The study found that the amount of Lactobacilli and glycogen level correlated strongly in both of the pre- and post-menopausal groups; i.e., as glycogen increased so too did the amount of Lactobacilli.
The research analyzed three vaginal Lactobacillus species: L. jensenii, L. crispatus, and L. iners. There was a correlation between glycogen levels with the presence of L. iners and L. jensenii. Yet, there was not a significant correlation of glycogen levels and L. crispatus. Concerning the difference of these species in pre- and post-menopausal women; pre-menopausal women had a trend to have more L. iners. L. jensenii and L. crispatus levels did not significantly differ between the pre- and post-menopausal women.
Concerning vaginal pH, there was a trend toward a more acidic vaginal pH in the samples from pre-menopausal women. The average pH of pre-menopausal samples was 4.0. Post-menopausal women’s vaginal fluid samples had an average pH of 4.6.
Clair Goodall: Author & Nature Lover
Clair Goodall is a bee-obsessed natural medicine convert from Minnesota. She is one expert you might want to know more about!
Clair will help you protect you and your family from toxic products and chemicals and help you discover solutions from nature.
Also, Clair’s book is backed by a 60-day, 100% money back guarantee
Visit Official Site!Natural Solutions for Yeast Infections after Birth Control Cessation

What might help you right away, is helping the vagina to be more acidic, and to introduce Lactobacilli bacteria into the vagina. To re-acidify the vagina, you can make a diluted apple cider vinegar (ACV) douche. You will not require much ACV to start healing a yeast infection. If you use undiluted ACV, the vaginal skin might become irritated and you can cause chemical burns in the area. Generally, you should stay under a 5% ACV concentration; e.g., use only 50 mL of ACV in liter of water. Research has indicated that even a 0.5% concentration of ACV might be enough to actually kill Candida cells; not just inhibit them. For more information on ACV and its use as an anti-Candida agent, you can find out more at this article: Apple Cider Vinegar for Yeast Infection.
In addition to acidifying the vagina, it may also be very helpful to reintroduce helpful probiotic Lactobacilli into the vagina. A very popular species, although not a normal inhabitant of the vaginal microbiome, L. acidophilus, might help to allay Candida infections; at least temporarily. In addition, many probiotic supplements for the digestive system have several species of Lactobacillus in them. If you can find one with L. jensenii, L. iners, L. gasseri, or L. crispatus; this might be very desirable to use in the treatment of your yeast infection.
Although L. acidophilus might not stay in the vagina too long; it could start assisting the natural Lactobacillus inhabitants of the vagina start to thrive by secreting lactic acid. It would probably be best to use a probiotic supplement with several species of Lactobacillus; especially the natural inhabitants of the vagina.
Once in the vagina, Lactobacilli bacteria can attach to areas on the vaginal wall; and thus prevent pathogens, like Candida, from attaching to these areas. Lactobacilli can also secrete beneficial chemicals like hydrogen peroxide (which Candida does not like) and bacteriocins (a protein toxin that is harmful to other bacteria).
For more information about using L. acidophilus for the treatment of a yeast infection; or using probiotic yogurt for this, you can find out more at the following articles:
A Natural, 12 Hour Solution for Yeast Infections

Yeast infections are certainly a ubiquitous health problem, affecting both men and women. Yet, women may be much more affected by Candida than men. Research published in Obstetrics & Gynecology [120.6 (2012): 1407-1414] stated that 75% of all women will develop a yeast infection at least one time in their lives. And, there are women that suffer very frequently from this health malady. According to the study, recurrent yeast infections affect about 5% to 8% of women throughout their reproductive years. The study also relates that recurrent yeast infections can bring about complications in sexual relations, costs, and intense suffering.
One woman who had to suffer through recurrent yeast infections was Linda Allen. Allen had more than an outward problem with Candida; she had a systemic problem with this yeast. Candida had overgrown in her body to the point it caused a host of unusual health problems; and, at the time, neither Linda or her doctor knew what was wrong with her. Linda was even put on allergy medication to solve her health issues; but nothing seemed to work.
Like many women, Linda went to the doctor when she first developed a yeast infection. Linda’s medical doctor prescribed her medication; and, she used it. The medication worked quite well at first; and, Linda found her yeast infection went away. Yet, it was not long before she developed another yeast infection. This problem, along with her terrible health issues, would plague Linda for about 12 years.
Eventually, Linda’s life finally took a turn for the better; this positive change happened when she visited a naturopath to address her terrible health. The naturopath was able to tell Linda exactly what was causing her unusual health problems and recurrent yeast infections: systemic Candidiasis. Although the naturopath did not give Linda a permanent solution, they did reveal the source of her problems.
Armed with the knowledge that Candida overgrowth was her body’s problem, Linda began to diligently study medical information. Linda read many books, tried several different purported treatments, and even inquired of medical professionals kind enough to lend her some time. Eventually, Linda would compile a natural treatment plan she hoped would effectively rid her body of Candida. In all, Linda would go on to spend about a year refining her new approach before she tried it on herself.
When Linda started her new treatment plan, she found that her recurrent yeast infections stopped; additionally, she found that her health was improving. Eventually, using her natural system, Linda was able to regain all her health; and become totally yeast infection free.
Linda showed her plan to a doctor and they said she might have something. The doctor suggested that Linda give her new system to others and see how they would respond. Linda decided to follow the doctor’s suggestion and gave her treatment plan to others who were suffering with Candida related health problems. Linda began hearing back from those who tried her system, and they too had experienced the same powerful results.
After getting free from systemic Candida, Linda decided to write a book detailing the natural system she used to regain her health. Linda’s book even contains an all-natural treatment plan that can be used to get rid of a yeast infection in only 12 hours. So, if you have a yeast infection somewhere on your body, Linda’s system can eliminate the symptoms of this problem in about half a day.
Linda has published her book with a large digital publisher; a subsidiary of Keynetics Incorporated (based in the United States). Linda’s publisher handles the ordering process and customer support for her book. And, Linda’s publisher provides a generous 60 day, 100% money back guarantee for her book. If you decide to try Linda’s treatment plan, and you find her book to be unsatisfactory, you can quickly get a full refund of your purchase quickly and easily. Keynetics makes sure your purchase is safe, easy, and provides customer support. Additionally, Linda’s book is available as an e-book; so you can download it immediately and start getting free from Candida right away.
To find out more about Linda’s personal journey to good health, see reviews of others who gave her book a try, or to learn more about her book; you can learn more at Linda Allen’s website.
Author: Mr. Nicholas Gross

Nick Gross is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Nick is primarily a web developer but also researches and authors written and video content about natural health. Nick has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Affiliate Disclosure
Some of the links provided on this website are affiliate links. When a purchase is made through these links, Candida Hub earns money from commission. This helps to keep the website up and helpful to people for free. Thank you for any support!
Stay Up to Date
If you enjoyed this article, consider following / liking our Facebook page. This page is primarily utilized to alert followers of new articles that are put on Candida Hub. Candida related news is also discussed. While you are there, you can see what has been more recently added to Candida Hub.
SOURCES:
- https://doi.org/10.1007/s00404-005-0740-4 — Murta, Eddie FC, C. A. Antoˆnio Filho, and Ana CM Barcelos. "Relation between vaginal and endocervical pH in pre-and post-menopausal women." Archives of Gynecology and Obstetrics [272.3 (2005): 211-213].
- https://doi.org/10.1007/s00404-005-0079-x — Farage, Miranda, and Howard Maibach. "Lifetime changes in the vulva and vagina." Archives of Gynecology and Obstetrics [273.4 (2006): 195-202].
- https://doi.org/10.3389/fmed.2018.00181 — Amabebe, Emmanuel, and Dilly OC Anumba. "The vaginal microenvironment: the physiologic role of lactobacilli." Frontiers in Medicine [5 (2018): 181].
- https://doi.org/10.1210/endo-76-1-63 — BITMAN, JOEL, et al. "Kinetics of in vivo glycogen synthesis in the estrogen-stimulated rat uterus." Endocrinology [76.1 (1965): 63-69].
- https://doi.org/10.1097/GME.0000000000000397 — Mirmonsef, Paria, et al. "An exploratory comparison of vaginal glycogen and Lactobacillus levels in pre-and post-menopausal women." Menopause [22.7 (2015): 702].
- https://doi.org/10.1097/AOG.0b013e31827307b2 — Marchaim, Dror, et al. "Fluconazole-resistant Candida albicans vulvovaginitis." Obstetrics & Gynecology [120.6 (2012): 1407-1414].