See all "Sex and Candida" Section Topics

Does it appear you seem to get a yeast infection after sex? Well, according to many different studies; and according to the seemingly general consensus among researchers; sexual intercourse does not change your odds of developing a vaginal yeast infection. One caveat to this is, of course, as long as your sex partner does not currently have a yeast infection. Yes, Candida fungi are contagious; and, sexual activity with someone with a Candida infection can lead to you getting an infection yourself (for more on this topic, you can check out Sex and Yeast Infection). Another caveat to this is oral sex and getting saliva on the vagina. Women who engage in frequently receiving oral sex, as evidenced by many studies, have a significantly increased risk for developing a yeast infection. Women who masturbate with saliva also have a significantly higher chance of developing a vaginal yeast infection.
So, again, no; sexual intercourse will not cause you to have a yeast infection. Vaginitis can be caused by many different microbes. Many women, when they feel itchy or burning sensations down there, quickly assume it is a yeast infection. This is typically not the case. Sexually transmitted diseases (STDs) also cause vaginal itching and burning. So, if you noticed your vagina seems to be infected after sex; you may have an STD—not a yeast infection. The symptoms of various STDs do tend to overlap; and, can often resemble a yeast infection. For more information about these symptoms of common STDs and yeast infections, you can check out Yeast Infections and STD’s.
If you’re a woman who is having sex with a man, and finds, for sure, a yeast infection occurs after sex; there is one thing you could do. A man’s semen is somewhat alkaline; with a pH of around 7.2 to 7.8. Candida do prefer a more alkaline environment; and a healthy vagina has a pH of around 4.5. So, when you have semen in the vagina, this can raise the vaginal pH. What you may find helpful, is washing out the semen from the vagina with diluted apple cider vinegar right away after sex. Just make sure you keep the concentration of the vinegar to about 1%. This should be strong enough to kill some Candida without causing harm. Strong concentrations of vinegar can cause the skin to become irritated or induce chemical burns (learn more about this vinegar here: Apple Cider Vinegar for Yeast Infection). This will help re-acidify the vagina and keep the pH low and unconducive to Candida overgrowth. This may help reduce the rate of recurrent yeast infections after sex. For a more complete, total solution to eliminate Candida fast (in about 12 hours), you can check out the last section of this article.
A 1/2 Day & Yeast is Gone!
Linda Allen suffered from yeast infections for years. Through researching natural medicine & Candida, she found an efficacious solution!
Linda is one expert you want on your side! Let her show you how to get rid of a superficial yeast infection in just 12 hours; AND, keep it gone!
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Research Findings

The first study we will examine was published in Epidemiology [7.2 (1996): 182-187]. The study was done on women at a university who were not pregnant and eligible for care at the college’s health services. Of the women who agreed to participate in the study, 64 served as clinical cases and 196 served as clinical controls. The clinical cases were women who had a positive vaginal laboratory culture for yeast. Case women all complained of at least one vulvovaginal symptom; and, most cases had signs consistent with vaginal Candidiasis. The clinical control women sought care for regular gynecological checkups, but they were not there for vulvovaginal symptoms. And, laboratory examination of their vaginal material was negative for yeast. Also, 431 women who responded to a mailed survey served as population controls.
The study found that 46.8% of the women with yeast infections had engaged in receptive oral sex two or more times in the previous two weeks. Compared to the control women, only 20.4% of them also had done this. As far as sexual intercourse was concerned, the odds of women having a yeast infection in the population control and case group were close to similar. The study concluded by stating that receptive oral sex, the use of oral contraceptives, spermicide use, and a prior diagnosis of vaginal yeast infection in the previous year were correlated with an increased risk for developing vaginal Candidiasis. Thus, sexual intercourse by itself, does not elevate the risk for a woman to develop vaginal yeast infection; but, receptive oral sex does carry a legitimate elevation of this risk.
Another study, published in the Australian and New Zealand Journal of Obstetrics and Gynaecology [47.4 (2007): 262-272], also related some findings regarding yeast infections and sex. The study shows that the general findings state that yeast infections do not result from sexual intercourse. The authors cite research showing the majority of women with recurrent vaginal Candidiasis, about 80% of them, have male sex partners that either do not have Candida or are slightly colonized by an entirely different species of Candida than the women had. Another paper, cited by the study, states that treating males had no effect on the rate of vaginal yeast infection occurrence in their female sex partners. Still another study, cited by this paper, explains that there was no difference in the rate of vaginal Candidiasis among women whose male partners were treated with an azole antifungal drug and women whose male partners received no such treatment. The authors conclude the following regarding sexual activity: “Expert consensus is that sexual transmission is not responsible for recurrent vulvovaginal Candidiasis, and partner treatment is not recommended unless symptoms are present.”

Another study, published in the Journal of Women's Health [12.10 (2003): 979-989], also discusses the role of sexual activity and recurrence of vaginal yeast infections. The study found, similar to other research, that there was a correlation between certain sex acts and yeast infections. As you may have guessed, a woman who receives oral sex is more likely to develop a yeast infection. Also women who masturbate with saliva, and women whose male partners masturbate with saliva, were also more likely to develop vaginal Candidiasis. The study suggests that the reason for this is due to the saliva’s ability to change the microbiota of the genitals and perhaps cause microtrauma. When the vaginal environment is altered via receptive oral sex, Candida may transform into its more virulent form; subsequently causing infection. The researchers also speculated that women without a history of recurrent Candidal vaginitis would be at less risk to develop a yeast infection, when they receive oral sex or masturbate with saliva. Lastly, the study found that the presence of Candida on the male partner was not a precursor to vaginal yeast infection. The study concludes by stating: “Sexual behaviors, rather than the presence of Candida species at various body locations of the male partner, are associated with recurrences of C. albicans vulvovaginitis.”
Another study, by the expert Dr. Jack Sobel, was published in the American Journal of Obstetrics and Gynecology [178.2 (1998): 203-211]. The study states that sexual intercourse has not been shown to change the rate of vaginal yeast infections. Women seem to start getting more yeast infections when they are regularly sexually active; in their 20’s. However, this correlation could indeed be spurious; and, it is not a clear indicator that sex causes Candidiasis. Yet, the study relates that frequent mouth to vagina contact does seem to increase a woman’s risk for genital Candidiasis.
Contraceptive Use and Yeast Infections

A study, published in the Journal of Obstetrics and Gynaecology [33.8 (2013): 850-856], examined the relationship between contraceptive use and vaginal yeast infections. The study used a total of 495 women; of them, 252 used contraceptives, and 243 did not use contraceptives. Using these two groups of women, the possible relationship between contraceptives and Candidiasis was analyzed. The contraceptive methods used among the women included the following:
- Menstrual Cycle Calendar Method and Coitus Interruptus (CCI)
- Oral Contraceptive Pills (OCP)
- Intrauterine Contraceptive Devices (IUCD)
- Condoms
- Unclassified
Concerning the various contraceptive methods, the occurrence of vaginal yeast infections did not differ much between the various methods. Yet, among these groups, vaginal Candidiasis occurred most frequently in the group of women who were taking oral contraceptives. And, vaginal Candidiasis was least likely in those women who used another (unclassified) method and not one of the primary methods articulated by the study. The researchers conclude the following regarding contraceptives: “Finally, our data also revealed that no contraceptive method predisposed women to vulvovaginal Candidiasis.”
Another study also examined the relationship of several behaviors to see if there was a positive correlation among them for vaginal yeast infections. The study was published in the journal Acta Obstetricia et Gynecologica Scandinavica [81.11 (2002): 1047-1052]. The study was conducted among 83 women who had a history of recurrent yeast infections. At the time when the women were tested for Candida, 43 tested positive and 40 tested negative. The study looked at 32 different parameters; among them was contraceptive use. The study cites that some research indicates that the use of estrogen birth control pills predisposes to yeast infection; but, this study did not show any strong correlation in this regard. No type of contraceptive use showed strong ability to predispose a woman to vaginal Candidiasis. One interesting thing the study did find, was that women who were were not positive for Candida had a higher rate of eating yogurt.
Another study also showed a slight indication that oral contraceptive pills do raise a woman’s chances of developing a yeast infection. The study was published in the journal Contraception [51.5 (1995): 293-297]. The study stated that oral birth control pills, with a high level of estrogen, are known to cause Candida species to proliferate more; however, birth control pills with a lower level of estrogen may not have the same effect. Regardless, the study states that women with recurrent yeast infections are commonly advised to discontinue such contraceptive pills. The study did not seem to find any hard evidence that birth control pills cause yeast infections, but they concluded with the feeling that they may in fact do.
Eliminate Bacterial Vaginosis & Vaginal Odor
Jennifer O’Brien is one prominent expert on BV that knows how to get rid of vaginal odor. BV is a common infection that you don’t have to put up with.
Jennifer will show you how to naturally eliminate vaginal odor in just 3 days.
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Conclusion
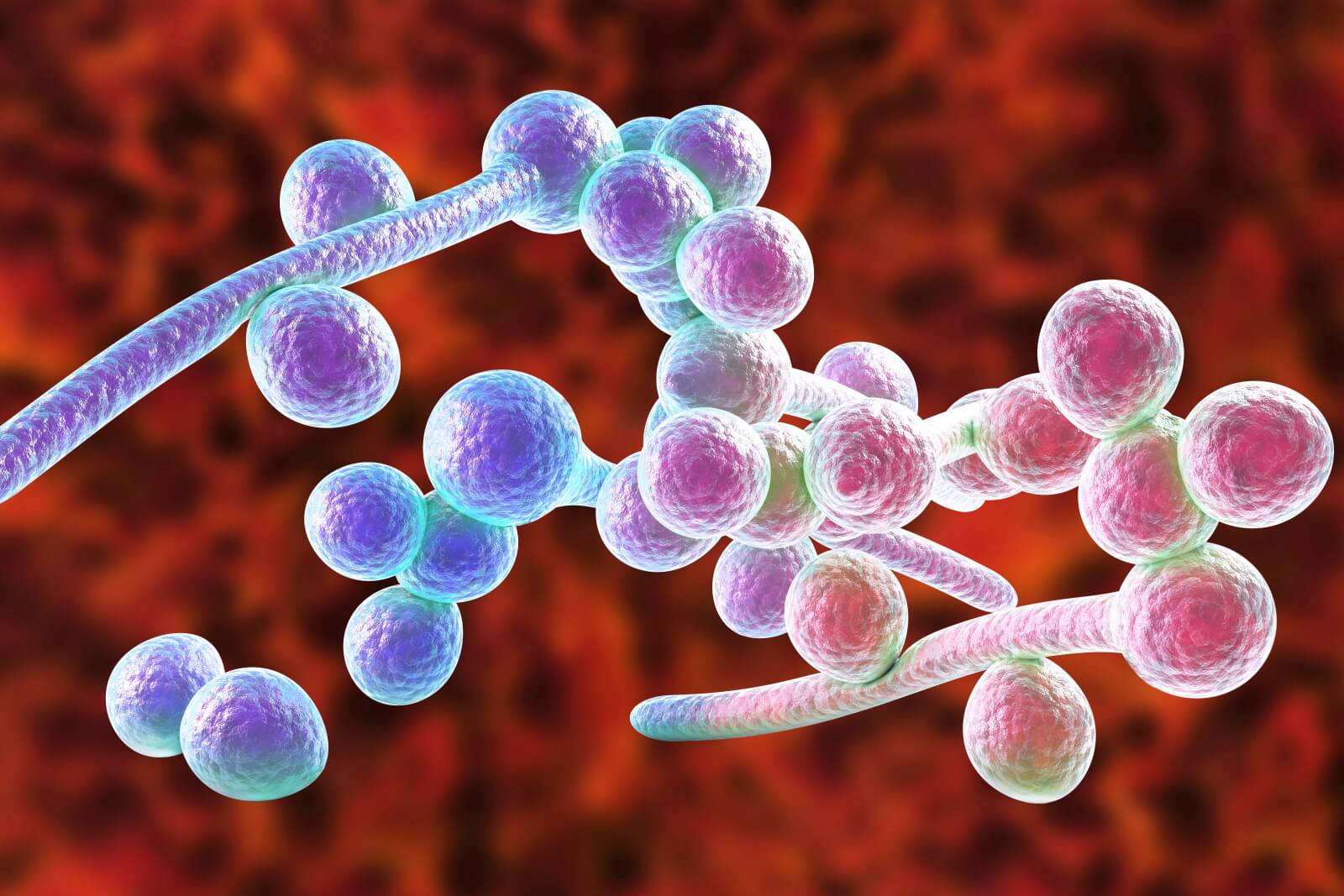
Given the aforementioned studies, we can see there is a clear pattern emerging. The presence of Candida in asymptomatic males does not elevate a female sex partner’s risk for Candidiasis. Oral contact, and saliva entering the vaginal area, both appear to increase the risk of yeast infections. Although, the presence of Candida in the mouth does not seem to be the primary reason for this phenomenon. Rather, it could be, that when the microbiotic life are disturbed by the introduction of saliva, and the vagina suffers microtrauma, this induces Candida to become more virulent. The result then may be, that frequent oral sex does tend to lead to more vaginal yeast infections. So, as long as your sex partner doesn’t have a yeast infection, sexual activities that do not involve saliva will be safer to engage in.
As far as birth control devices used, these do not seem to influence the occurrence of a yeast infection; with one possible exception: intrauterine device (IUD) use. Studies have indicated that Candida can attach to these devices; and, thus, may cause an infection. Some instances of recurrent vaginal Candidiasis have been resolved through the removal of IUDs. However, the risk for getting Candida because of an IUD, may not be too steep. So, your use of a condom or spermicide does not appear to be able to bring about a yeast infection after sex. Since both sexual intercourse and birth control protocols (excluding estrogen based birth controls; and, probably, IUDs as well) do not seem to affect the rate of Candidiasis, they are likely not going to be the cause of a yeast infection after sex. Remember, since STDs are similar in their symptoms, many women mistake them for a yeast infection!
Clair Goodall: Author & Nature Lover
Clair Goodall is a bee-obsessed natural medicine convert from Minnesota. She is one expert you might want to know more about!
Clair will help you protect you and your family from toxic products and chemicals and help you discover solutions from nature.
Also, Clair’s book is backed by a 60-day, 100% money back guarantee
Visit Official Site!12 Hour Holistic Yeast Infection Cure

As you may know, some women develop a severe problem with Candida; frequently getting yeast infections again and again. One woman who lived this everyday hell, and had her overall health greatly diminished, was Linda Allen. Linda’s Candida problem began to emerge in her late teen years. When she was diagnosed with a sinus infection, she also found herself coming down with a yeast infection. When Linda figured out it was a yeast infection, she went quickly to a medical doctor to get a prescription treatment. And, it worked seemingly easy enough; however, a short while later the yeast infection came back. Again, Linda saw her physician and got another prescription. Like before, the Candida overgrowth in her vagina recurred yet again shortly after she got it cleared up. This cycle of yeast infection occurrence, and subsequent treatment, seemed like a never ending story.
All the while she battled the vaginal infections, Linda’s overall health was continuing to worsen. She went to the doctor so much those who knew her wondered if she was a hypochondriac or just sicker than she was letting on! Despite her doctor prescribing stronger and stronger antibiotics for her symptoms, Linda never seemed to get better for long. Linda’s poor health and frequent yeast infections plagued her life for more than a decade. Until, she went to a naturopath and was told her problem was really a systemic Candida infection. The abundance of yeast in her body was leading to her poor health and frequent vaginal maladies. Yet, despite the help from the naturopath, Linda didn’t seem to find a permanent solution. Even Candida diet plans only worked while she adhered to the strict guidlines; her poor health would come right back after she stopped eating the right way.
Around this time, Linda decided to find any answers she could herself. Determined, Linda began reading books and medical information relating to Candida. And, when any doctor or natural medicine expert would be kind enough to give her some time, Linda consulted them for further information. In the course of 12 years of studying, Linda also tried a wide array of natural and alternative therapies to solve her Candida problem. Although none of this helped stop her yeast infections, she did pick up valuable clues that would later help her.
As Linda began to see the need to address the root causes of Candidiasis, she began to put together key information she had learned. As time went on, Linda developed a new approach to totally curing her Candida problem. Linda spent about a year polishing and refining her technique; and, when she put it into practice on herself she was stunned. Quickly, her vaginal yeast infections disappeared. And, as time went on, they stayed gone. Also, the horrible health she had suffered with also started to improve. It wasn’t long before the fatigue and other symptoms of excessive Candida overgrowth evaporated—never to return!
Linda has since published her findings in a sophisticated, comprehensive book. Since Linda published her book in 2004, she has seen over 100,000 people from all over the world get free of their Candida struggles for good. And, she has helped men and women get rid of their yeast infections in just 12 hours time. Linda’s step by step approach to correcting the underlying causes of Candida has dramatically changed the lives of many people.
Linda Allen has published her book with one of the largest online retailers in the world; which is owned by the large U.S. based company Keynetics Incorporated. Linda’s book is offered in digital format (PDF), and can be accessed instantly, if you decide to check it out. Linda also knows the disappointment of trying a cure only to find it doesn’t live up to expectations; and, so offers a 60 day, 100% money back guarantee. So, if your try Linda’s book, and find your yeast infection isn’t gone in 12 hours; or, that your systemic yeast infection isn’t resolved in a few weeks, you can quickly get all your money back.
If you would like to learn more about Linda’s personal story and journey to better health, see some of the extra books she offers with her publication, or see several testimonies of others who used her book, you can find out more information at Linda Allen’s website.
Author: Mr. Nicholas Gross

Nick Gross is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Nick is primarily a web developer but also researches and authors written and video content about natural health. Nick has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Affiliate Disclosure
Some of the links provided on this website are affiliate links. When a purchase is made through these links, Candida Hub earns money from commission. This helps to keep the website up and helpful to people for free. Thank you for any support!
Stay Up to Date
If you enjoyed this article, consider following / liking our Facebook page. This page is primarily utilized to alert followers of new articles that are put on Candida Hub. Candida related news is also discussed. While you are there, you can see what has been more recently added to Candida Hub.
SOURCES:
- http://www.jstor.org/stable/3703033 — Geiger, Ann M., and Betsy Foxman. "Risk factors for vulvovaginal candidiasis: a case-control study among university students." Epidemiology 7.2 (1996): 182-187. PubMed
- http://dx.doi.org/10.1111/j.1479-828X.2007.00736.x — Watson, Cathy, and Helen Calabretto. "Comprehensive review of conventional and non?conventional methods of management of recurrent vulvovaginal candidiasis." Australian and New Zealand journal of obstetrics and gynaecology 47.4 (2007): 262-272. PubMed, PDF Available Here
- http://dx.doi.org/10.1089/154099903322643901 — Reed, Barbara D., et al. "Candida transmission and sexual behaviors as risks for a repeat episode of Candida vulvovaginitis." Journal of Women's Health 12.10 (2003): 979-989. PubMed, PDF Available Here
- http://dx.doi.org/10.1016/S0002-9378(98)80001-X — Sobel, Jack D., et al. "Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations." American journal of obstetrics and gynecology 178.2 (1998): 203-211. PubMed
- http://dx.doi.org/10.3109/01443615.2013.834306 — Güzel, A. B., et al. "Candida vaginitis during contraceptive use: the influence of methods, antifungal susceptibility and virulence patterns." Journal of Obstetrics and Gynaecology 33.8 (2013): 850-856. PubMed
- http://dx.doi.org/10.1034/j.1600-0412.2002.811109.x — Novikova, Natalia, and Per?Anders Mårdh. "Characterization of women with a history of recurrent vulvovaginal candidosis." Acta obstetricia et gynecologica Scandinavica 81.11 (2002): 1047-1052. PubMed
- http://dx.doi.org/10.1016/0010-7824(95)00079-P — Spinillo, Arsenio, et al. "The impact of oral contraception on vulvovaginal candidiasis." Contraception 51.5 (1995): 293-297. PubMed