See all "Sex and Candida" Section Topics

Is there a relationship between sex and a yeast infection? The answer is certainly “yes.” Research has even stated, that Candida has potential as a biological weapon due to its communicability! According to the United States’ MedlinePlus article, yeast infections are not usually contagious; but can spread.
People who are at the greatest risk, as you may have guessed, are those with a weakened immune system. Many different studies conducted also show, that sexual activity with a partner who is infected with Candida, can result in the yeast being spread to the uninfected individual.
Some research indicates that the odds of you developing a yeast infection, from an infected sex partner, can perhaps be over 10%; and, even potentially be as high as about 38%. So, the conclusion of the matter is, that having sex with a person with a genital yeast infection is risky. Yes, you probably won’t get infected by doing it; however, there is a very real chance you will pick up the infection during sex.
Some sexual acts, as research indicates, also seem to increase the odds of a woman developing a yeast infection. The primary sex act linked to recurrent infections is a women receiving oral sex. Also, a male sex partner who masturbates with saliva also appears to increase the odds of their female partner getting a yeast infection.
It is, therefore, perhaps the saliva coming into contact with the female’s vagina that imputes the risk to this sex act. Although you may think that trace amounts of Candida on the penis or in the male’s semen is responsible for increased yeast infection recurrence; research indicates that this is not the case.
The presence of trace amounts of Candida on the male partner does not seem to induce recurrent female Candidiasis. Many studies are listed in the sources of this article; feel free to peruse them for greater detail about these issues.
If you are looking to get rid of a Candida problem fast, you can check out the various natural remedies on Candida Hub. Essential oils, coconut oil, honey, and medicinal herbs are all powerful natural alternatives to expensive, artificial, prescription drugs.
There is a lot of information about these therapies you can check out at your convenience. If you want to learn about one of the fastest; and most effective ways to get rid of your Candida problem in 12 hours; you can find out more at the close of this article.
A 1/2 Day & Yeast is Gone!
Linda Allen suffered from yeast infections for years. Through researching natural medicine & Candida, she found an efficacious solution!
Linda is one expert you want on your side! Let her show you how to get rid of a superficial yeast infection in just 12 hours; AND, keep it gone!
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Sex and Candidiasis Research

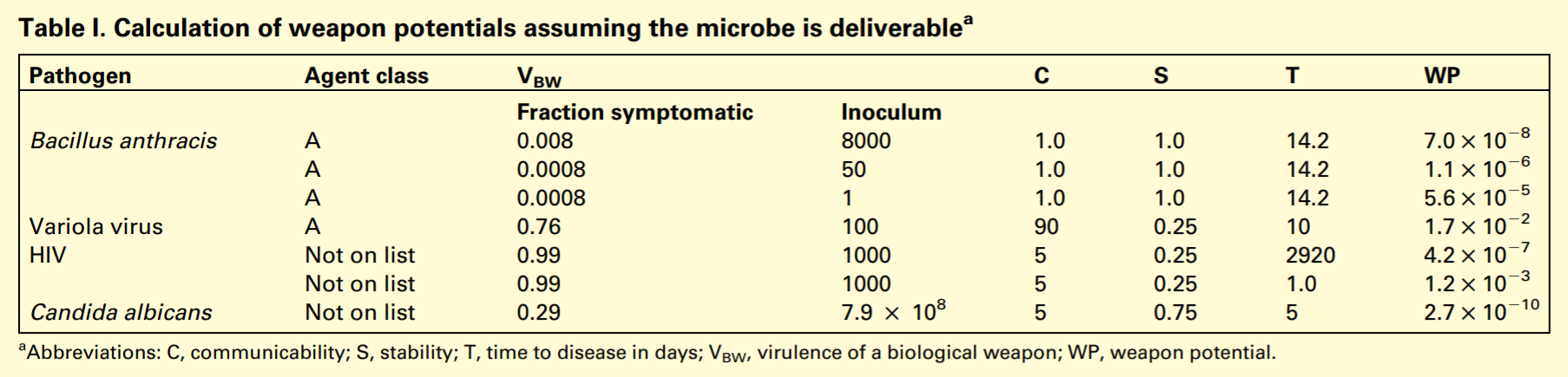
The first study we will look at is quite interesting; and, is entitled The Weapon Potential of a Microbe. The study, published in Trends in Microbiology [12.6 (2004): 259-263], sought to classify various microorganisms by their potential to be used as biological weapons.
And, Candida albicans, the species of Candida which causes around 80% of all Candida infections (and the most virulent of the Candida genus) (Fidel, et al.; 1999), was included in the study.
The study used a formula to describe the weapon potential of an infective agent; the formula is as follows: WP = VBWSC / T. WP stands for “weapon potential;” and, this is equal to the virulence of a biological weapon (VBW) multiplied by organism stability (S), multiplied by organism communicability (C), divided by the time (T) it takes to cause damaging infection.
In the study, the VBW assessment of a microbe was done by considering the amount of symptomatic infections versus the amount of asymptomatic infections resulting from a given inoculum (inoculum = the amount of a pathogen released into the body). And, by these reasonable standards, Candida had a very real degree of virulence.
The study stated that there is evidence a mother can transmit Candida to her child during birth; and, that sexual transmission can possibly occur. Thus, because of the unlikely possibility Candida will be transmitted via contact, they set the communicability score of this organism to a low value of 5.
The human immunodeficiency virus (HIV), was also given a low communicability score of 5, as well. Virulence was determined by considering the amount of symptomatic cases a specific amount of the pathogen would induce.
Candida’s virulence was one of the lowest among the organisms in the study. The stability of Candida was set to a higher value than HIV; and, time to infection was set at 5 days.
Thus, the total weapon potential of Candida was somewhat similar to HIV. So, yes, according to this research, yeast infections are certainly communicable and can be transferred during contact. And, since many yeast infections attack the genitals or mouth, sexual activity can easily bring about the direct contact required to spread this yeast.
Below is a chart, taken from the study, showing the results of the study’s calculations for a few pathogens; among them is Candida albicans.
The next study we will investigate, was published in the African Journal of Microbiology Research [3.11 (2009): 694-699]. The study relates that the CDC has stated Candida can make it easier for other STD’s to be transmitted.
As far as if a yeast infection is contagious; the answer, according to this study, is certainly "yes." Due to this pathogen being contagious, the study explains that Candida can be sexually transmitted.
In fact, the study cites research and states sexual intercourse is the most common mode of infection for genital Candidiasis. The following quote, about yeast infections and their propensity to spread during sex, was taken from this study:
Candida is found in the vagina of 35 - 50% of healthy women. Under some conditions, such as reduced immunity, prolonged antibiotics therapy, use of contraceptives, malnutrition, pregnancy, diabetes, obesity, tissue transplant, use of immunosuppressive drugs (Corticosteroids), neutropenia, Candida may become pathogenic and cause candidiasis (Okungbowa et al., 2003).Presence of indwelling central venous or pulmonary artery catheters and prior hemodialysis has also been identified as a risk factor (Barg, 1993). Sexual intercourse with an infected person is the most common mode of spread of genital candidiasis (Ogunbayo, 1988; Tatfeng et al., 2004).
http://academicjournals.org/journal/AJMR/article-stat/B5182DA14604
Another research study, published in Vojnosanitetski Pregled [67.10 (2010): 819-824], also looks at sexual activity; and, if it could be a predisposing factor in vaginal yeast infections. The study states that yeast infections can spread during sexual activity. However, as far as sex alone being responsible for an outbreak of Candida, the study showed this is not true.
The rate of sexual activity in the control group (a group of women with a low rate of vaginal Candidiasis), and the rate of sexual activity in the test group (women with 4 or more episodes of vaginal Candidiasis in the last year), were very similar. Thus, the research shows that the amount of sex a woman has does not in any way determine her susceptibility to vaginal yeast infections.
The next study, published in Critical Reviews in Microbiology [37.3 (2011): 237-244], discusses the relevance of the penis being a reservoir for Candida to reinfect a sex partner’s vagina. The study cites research demonstrating that men who have sex with a woman with a vaginal yeast infection, around 10% to 38% of them, will develop a penile yeast infection.
And, there is research demonstrating that the female partners of men with penile yeast infections have a higher rate of vaginal Candidiasis. The paper also points out two studies that show Candida can be sexually acquired.
Even a skeptical study found that, in 64 different sexually active couples—where one partner had a genital yeast infection—17.2% of the couples had genetically identical strains of Candida. Although Candida can be spread sexually, it is likely that sexual intercourse is not an important factor behind recurrent vaginal Candidiasis.
Eliminate Bacterial Vaginosis & Vaginal Odor
Jennifer O’Brien is one prominent expert on BV that knows how to get rid of vaginal odor. BV is a common infection that you don’t have to put up with.
Jennifer will show you how to naturally eliminate vaginal odor in just 3 days.
A 60-day, 100% money back guarantee is provided.
Visit Official Site!Oral Sex and Yeast Infection
One study did find a slight correlation with vaginal yeast infections and the amount of oral sex women receive. The study was published in the Journal of Women's Health & Gender-Based Medicine [9.6 (2000): 645-655]. The study used 156 women with vaginal Candidiasis and 92 women serving as controls (these women had been without a vaginal yeast infection for at least a year).
The study found women who had more receptive oral sex had a slightly increased chance of getting a vaginal yeast infection. Women who reported receiving oral sex five times or more a month; had an even higher rate of vaginal yeast infections. Another slight risk factor, was knowing a sexual partner for a shorter period of time.
Another study, published in the Journal of Women's Health [12.10 (2003): 979-989], looked at 148 women with vaginal yeast infections and 78 of their male sex partners. The study found that women who practiced receptive oral sex, also had an increased risk of developing vaginal Candidiasis.
The study found that women who received oral sex during the last month had a 27.8% recurrence rate; compared to a 11.6% recurrence rate among women who did not receive oral sex in the past month. Also, women who masturbated with saliva, also had close to a three fold increase in their chances for developing a vaginal yeast infection.
As far as the presence of Candida in the male’s genitals; this did not have any effect on the rate of yeast infection recurrence. The study concluded, that sexual behaviors—not the presence of Candida on various locations of the male partner—were associated with recurrent vaginal Candidiasis.
The study did not seem to say much about the male partners having a symptomatic (apparent) candida infection; thus, the presence of Candida in various locations on the males’ bodies is assumed to be non-pathogenic. The semen of men can rarely have yeast, and Candida specifically, in it (Huyser, C., et al.; 1991).
A study that looked at 198 different women; who attended genitourinary clinics in London, Loughborough, and Leicester; found that 179 of these 198 women had some form of Candida (present in two or more body locations) in their bodies (Odds, F. C., et al.; 1989).
Putting this issue most blatantly, was a study published in Trends in Microbiology [21.7 (2013): 334-341]. The study states that the typical rate of yeast colonizing the body among healthy adults (those without yeast infections) ranges from approximately 30% to 70%.
The authors of this study state: “...Candida and Malassezia can be found at significant levels on mucosal surfaces and the skin, even in healthy hosts, and it is from within their niche in the microbiome that they can cause disease.” Thus, given these facts, it is easy to assume the 78 male partners of women in the Journal of Women's Health [12.10 (2003): 979-989] study, did not have active infections for the most part; but, rather this study merely found that Candida was to some extent living in these men’s bodies. Which, according to other scientific investigation, is very normal for healthy individuals.
Clair Goodall: Author & Nature Lover
Clair Goodall is a bee-obsessed natural medicine convert from Minnesota. She is one expert you might want to know more about!
Clair will help you protect you and your family from toxic products and chemicals and help you discover solutions from nature.
Also, Clair’s book is backed by a 60-day, 100% money back guarantee
Visit Official Site!Contraceptive Use & Candida
A study, published in 1970, looked at the relationship between women using oral contraceptives and Candida infections. The study was published in Acta Obstetricia Et Gynecologica Scandinavica [Volume 49 (3) - Jan 1, 1970]. One thing to remember, is that formerly Candida albicans classification encompassed more than just the species we refer to as Candida albicans today. However, this detail should not be of much importance.
The study utilized 276 healthy women who were of reproductive age. These women were divided into three groups: Group P, consisted of 80 women who used oral contraceptives. Group NP, consisted of 158 women who did not use oral contraceptives.
And, a third group, Group AP, consisted of 38 women who formerly used oral contraceptives. The average ages of the women in these three groups were: 32 years for group P, 37 years for group NP, and 32 years for group AP.
All of the women participating in the study had gynaecological exams performed on them; vaginal swabs were taken and examined by microscopic culturing. A vaginal test for trichomoniasis was also conducted, and a case history was ascertained.
The study found that the occurrence of Candida albicans in the vagina was higher in users of oral contraceptives. Of the women who used oral contraceptives, 15% tested positive for Candida albicans.
Of the women who did not use oral contraceptives, 5% tested positive for this yeast. The study stated that the difference was significant (likely not due to chance) at the 5% level. Therefore, it appears there is more of a risk for having Candida when you use contraceptives.
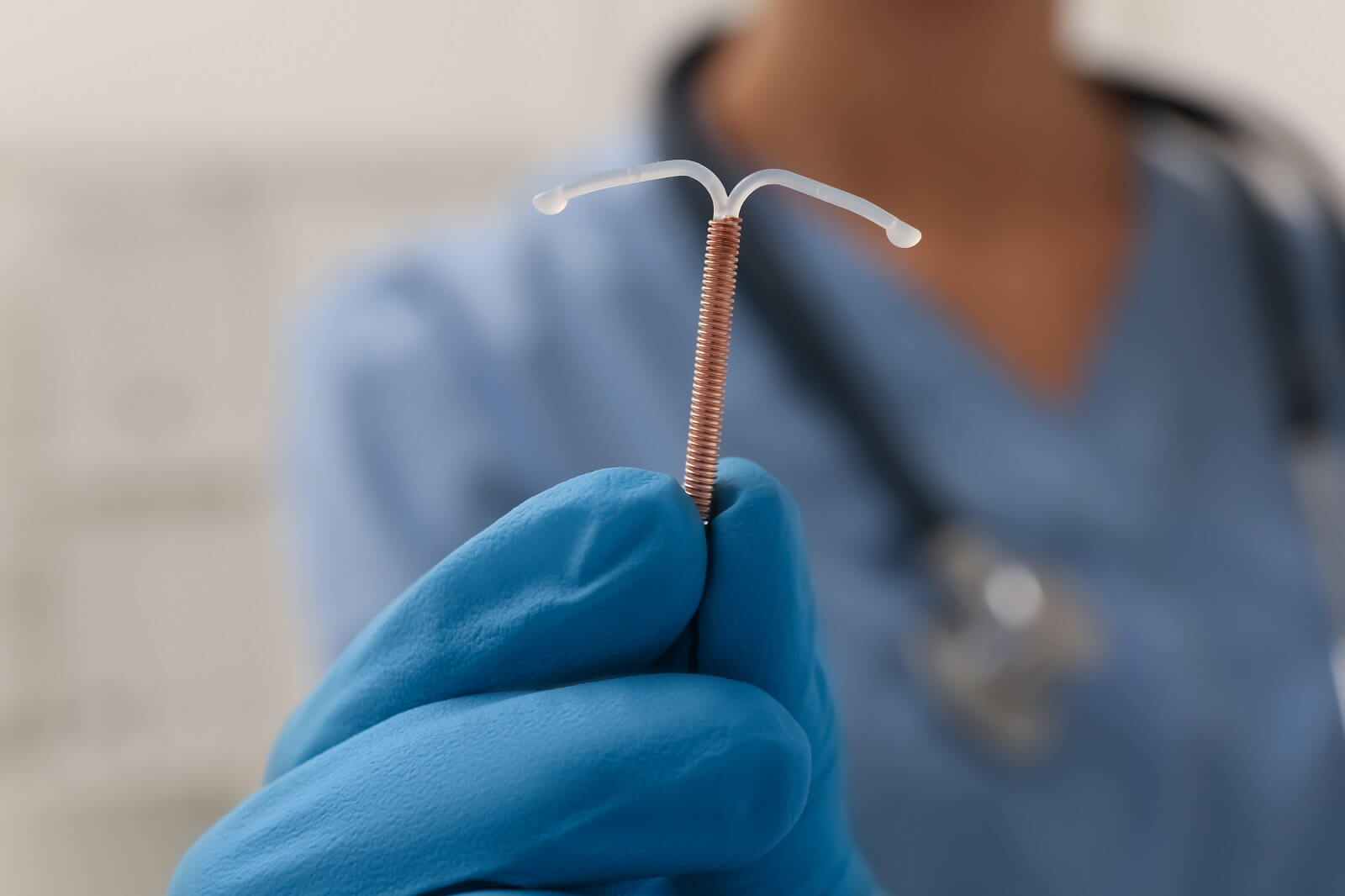
Concerning the use of an intrauterine device (IUD), a study examined how Candida could colonize these devices. The study was published in Contraception [Volume 77 (5) - May 1, 2008]. The study used two different isolates of Candida albicans; and, sought to see how they would grow on an IUD. The research found that all the yeast cells evaluated in the study showed a high ability to develop biofilm.
Biofilm is a thick sludge that covers yeast cells; and imparts greater protection to the cells. It can also greatly increase the cells’ resistance to antifungal drugs (Khan, et. al; 2012).
This research found that the yeast cells could adhere to all the parts of the IUD. The study suggested that the adherence of Candida albicans to the IUD, and its formation of biofilm, appears to be important factors influencing the development of vaginal yeast infections, and repeat occurrences of these infections.
The study also makes clear that 5% of the women who develop a yeast infection will suffer from repeat vaginal yeast infections. And, recurrent vaginal Candidiasis has been stopped via the removal of IUDs. The study also cited another study, which stated IUD users have significantly more yeast cells in their vaginas than non-users do.
IUD users have a 20% Candida colonization rate; and, non-users have a rate of 6%. The following quotation, regarding this, was taken from the study:
Parewijck et al. showed that IUD users have significantly more yeast cells in the vagina (20%) than nonusers (6%). These studies confirm the clinical impression that the IUD predisposes to colonization and infection by yeast cells and VVC [vulvo-vaginal Candidiasis] or RVVC [recurrent vuvlvo-vaginal Candidiasis] development.
Contraception [Volume 77 (5) - May 1, 2008]
Concerning condoms, and if they can instigate a yeast infection, the answer is no. Although condoms do not cause yeast infection, if you would like to learn more about this, there is an entire article explaining this. For more information, feel free to check out: Can Condoms Really Cause Yeast Infections?.
Conclusion

Yes, a yeast infection on any part of the body is contagious; and, sex with an infected partner can result in you getting a yeast infection. Although the transmission is somewhat rare, there is still perhaps over a 10% chance that your sexual activity with an infected partner will result in a yeast infection.
Also, the presence of trace amounts of Candida on the male penis or semen does not seem to be a causative factor for a female sex partner to develop a yeast infection. Rather, sex acts like women receiving oral sex, that put the saliva directly onto the vagina, seem to be the primary sexual activity risk factor for vaginal Candidiasis; as many studies state.
The Journal of Women’s Health [12.10 (2003): 979-989] study suggested that oral sex and saliva on the genitals may disrupt the normal microbiome of that area, thus leading to increased incidence of yeast infections. This study states the following:
Previous study of the immunopathogenesis of recurrent Candida vulvovaginitis suggests that a delicate equilibrium exists among C. albicans, vaginal bacterial flora, and vaginal defense mechanisms, and that changes in the host environment promote the transformation of C. albicans from a saprophytic to a pathogenic existence.
We suggest that the effects of genital washing with saliva—from either the male or the female—might upset this balance, either by upsetting the normal surface environment by saliva or by microtrauma mechanisms or by the introduction of immunological elements, stimulants, or modifiers that cause an altered environment that promotes the development of symptomatic recurrent Candida vulvovaginitis.
http://dx.doi.org/10.1089/154099903322643901
Linda Allen’s 12 Hour, Natural Candida Cure

Linda Allen was one of many unfortunate people who lived with a systemic Candida problem for years. Besides routinely getting vaginal yeast infections, the other symptoms of this condition—such as fatigue, bacterial infections, heartburn, etc.—also plagued Linda’s life. The start of Linda’s Candida problems began in her late teen years, after developing a sinus infection.
Shortly thereafter she developed a vaginal yeast infection. Initially Allen went to a physician for a prescription treatment for her yeast infection; and, at first it worked. Yet, it was only a short while before her infection returned.
She again went to her doctor for another prescription; however, like before, the Candida came quickly back after it was cleared up. During this time her health worsened and she was prescribed stronger and stronger antibiotics.
Yet, nothing seemed to work, and the drugs never seemed to solve her problem.
This cycle of yeast infection recurrence and poor health would continue to torment Linda for over a decade. She regularly suffered from all the pains a yeast infection brings with it; despite using a myriad of prescription medications and over the counter treatments.
Nothing seemed to work. Linda then decided to try and find answers to her problem herself; hoping that there was some solution out there to find.
After a naturopath pointed out that her health issues were due to a systemic Candida problem, she finally had a starting point. Linda spent the next 12 years devouring information on holistic medicine. She thoroughly read many pertinent health books, did ardent medical research, and picked the brains of any naturopath or medical doctor kind enough to lend her their time.
Linda also tried many different alternative therapies that promised a solution to her problem; yet, none permanently ended her Candida crisis.
Finally, after deciding she needed to address the root causes of Candida overgrowth in her body, she began to make some connections. With all her experience and study in this area, she started to see how to possibly control the underlying physiological issues that predisposed her to Candida overgrowth. She spent a year polishing and adjusting this new approach; and, when she tried it, she found she was rapidly cured of her yeast infection.
As the weeks went on, she kept following her 5 step approach. Thankfully, her research and effort had paid off—as time kept going on, weeks turned into months and the Candida stayed gone. Her previously horrible health rapidly improved with each day, and she felt like a new woman!
Since finding a natural system to treat Candida problems, Linda has gone on to write a detailed book explaining how to exactly copy her success.
Since her book was published in 2004, over 100,000 people from around the world have seen the same success Linda did. Linda Allen’s book is one of the most popular, and effective, books that gives a permanent solution for even stubborn, systemic Candida problems.
Linda Allen’s book is published and sold by one of the largest online retailers, owned by the large U.S. based firm Keynetics Incorporated. Linda also knows how hard it is to be hopeful of a solution and be let down; and, offers a 60 day, 100% money back guarantee on her book.
If you try her book and find your yeast infection isn’t cleared up in 12 hours, or the systemic yeast in your body isn’t gone in a few weeks, you can quickly get a full refund. Also Linda Allen provides a few bonus books for free along with her book; you may want to check these out too!
If you’d like to see testimonies of other people who gave Linda’s book a try, learn more about Linda Allen’s personal journey to yeast infection freedom, or learn about the bonus books she offers, you can find out more information at Linda Allen’s website.
Author: Mr. Nicholas Gross

Nick Gross is a natural medicine enthusiast who has been researching and writing about natural medicine since 2008. Nick is primarily a web developer but also researches and authors written and video content about natural health. Nick has a bachelor’s degree in Management Information Systems from the University of Northern Iowa.
Disclaimer
The information on this website is not a prescription for anyone. This information is for informational or educational purposes only, and is not a substitute for professional medical advice or consultations with healthcare professionals.
Affiliate Disclosure
Some of the links provided on this website are affiliate links. When a purchase is made through these links, Candida Hub earns money from commission. This helps to keep the website up and helpful to people for free. Thank you for any support!
Stay Up to Date
If you enjoyed this article, consider following / liking our Facebook page. This page is primarily utilized to alert followers of new articles that are put on Candida Hub. Candida related news is also discussed. While you are there, you can see what has been more recently added to Candida Hub.
SOURCES:
- https://www.nlm.nih.gov/medlineplus/ency/article/000880.htm — U.S. National Library of Medicine’s MedlinePlus article on Candidiasis.
- http://dx.doi.org/10.1016/j.tim.2004.04.007 — Casadevall, Arturo, and Liise-anne Pirofski. "The weapon potential of a microbe." TRENDS in Microbiology 12.6 (2004): 259-263. PubMed
- http://www.ncbi.nlm.nih.gov/pubmed/9880475 — Fidel, Paul L., Jose A. Vazquez, and Jack D. Sobel. "Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans." Clinical microbiology reviews 12.1 (1999): 80-96. PubMed Full Text
- http://academicjournals.org/journal/AJMR/article-stat/B5182DA14604 — Akortha, E. E., V. O. Nwaugo, and N. O. Chikwe. "Antifungal resistance among Candida species from patients with genitourinary tract infection isolated in Benin City, Edo state, Nigeria." African Journal of Microbiology Research 3.11 (2009): 694-699. PDF Available Here
- http://dx.doi.org/10.2298/VSP1010819J — Jankovi?, Slobodan, et al. "Risk factors for recurrent vulvovaginal candidiasis." Vojnosanitetski pregled 67.10 (2010): 819-824. PubMed, PDF Available Here
- http://dx.doi.org/10.3109/1040841X.2011.572862 — Aridogan, Ibrahim Atilla, Volkan Izol, and Macit Ilkit. "Superficial fungal infections of the male genitalia: a review." Critical reviews in microbiology 37.3 (2011): 237-244. PDF Available Here, PubMed
- http://dx.doi.org/10.1089/15246090050118170 — Reed, Barbara D., et al. "Sexual behaviors and other risk factors for Candida vulvovaginitis." Journal of women's health & gender-based medicine 9.6 (2000): 645-655. PubMed, PDF Available Here
- http://dx.doi.org/10.1089/154099903322643901 — Reed, Barbara D., et al. "Candida transmission and sexual behaviors as risks for a repeat episode of Candida vulvovaginitis." Journal of Women's Health 12.10 (2003): 979-989. PubMed, PDF Available Here
- http://dx.doi.org/10.1007/BF01139781 — Huyser, C., et al. "Microbial flora in semen during in vitro fertilization."Journal of in vitro fertilization and embryo transfer 8.5 (1991): 260-264. PubMed
- http://dx.doi.org/10.1099/00222615-29-1-51 — Odds, F. C., et al. "Candida species and C. albicans biotypes in women attending clinics in genitourinary medicine." Journal of medical microbiology 29.1 (1989): 51-54. PubMed
- http://dx.doi.org/10.1016%2Fj.tim.2013.04.002 — Huffnagle, Gary B., and Mairi C. Noverr. "The emerging world of the fungal microbiome." Trends in microbiology 21.7 (2013): 334-341. PubMed Full Text
- https://doi.org/10.3109/00016347009157254 — Incidence of Candida Albicans in Women Using Oral Contraceptives. Acta Obstetricia Et Gynecologica Scandinavica [Volume 49 (3) - Jan 1, 1970]
- https://doi.org/10.1016/j.contraception.2008.01.007 — Chassot, Francieli; et. al. Can intrauterine contraceptive devices be a Candida albicans reservoir? Contraception [Volume 77 (5) - May 1, 2008]
- http://dx.doi.org/10.1016/j.jep.2012.01.045 — Khan, Mohd Sajjad Ahmad, and Iqbal Ahmad. "Biofilm inhibition by Cymbopogon citratus and Syzygium aromaticum essential oils in the strains of Candida albicans." Journal of ethnopharmacology [140.2 (2012): 416-423].